Hey all, it is Coach Tyler here!
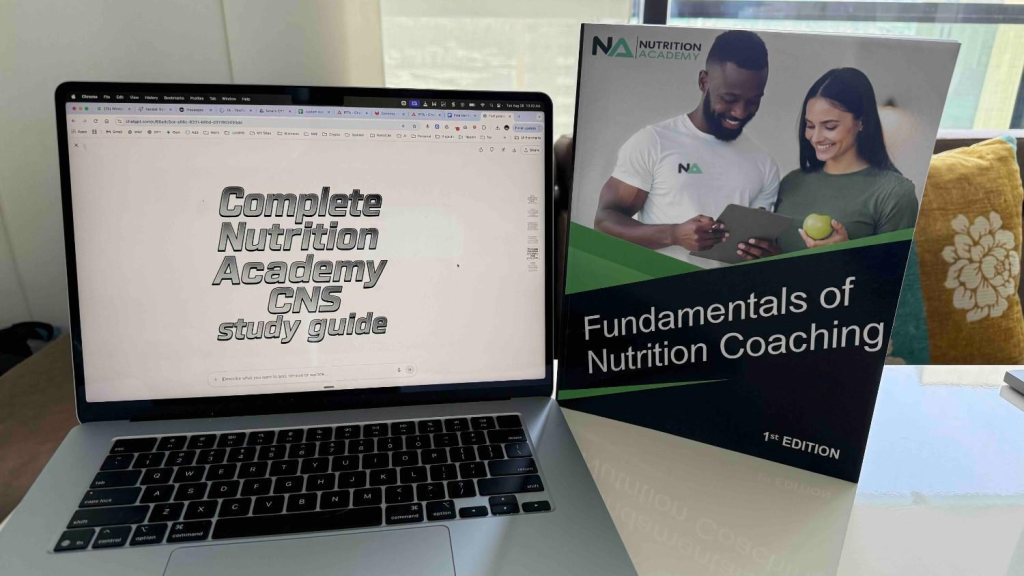
Welcome to the Free Nutrition Academy CNS study guide from PTPioneer. I have crafted this guide for students to concisely learn all that they can about the most important topics within the International Personal Trainer Academy’s nutrition specialization and certification.
This IPTA Nutrition Academy CNS guide accompanies the textbook that you can get for free here with the trial. IPTA often runs a buy-one-get-one deal that includes CPT and Nutrition.
The study guide below covers these items:
- A breakdown of each of the 26 chapters within the Nutrition Academy CNS certification textbook.
- Study tips focusing on what it takes to pass the exam.
- Some ideal ways to combine this guide with the official study materials
Nutrition Academy CNS Study Series
- Nutrition Academy CNS Study Guide
- Nutrition Academy CNS Practice Exam
- Nutrition Academy CNS Flashcards
Free Nutrition Academy CNS Study Guide Updated for 2025
Before starting the study guide, you should know that the IPTA offers a study plan focused on getting you exam ready within 4 weeks. This plan includes the use of tailored studying and online study materials all done at your own pace. You can also sign up for a free trial and get a free copy of the Nutrition Academy CNS textbook.
These materials also partner perfectly with the IPTA CPT Program and includes an Exam Pass Guarantee.
The IPTA will cover all that is needed for getting you to pass your certification program on the first try. It also partners well with this free guide, if you want to start here to get a sample of the topics that will be covered in this program.
The Nutrition Academy CNS certification goes beyond facts—it builds real-world coaching skills to help clients succeed. Sometimes the IPTA runs a buy one get one BOGO deal which includes the IPTA CPT at no extra cost, giving you a certification in training and nutrition at an amazing cost. At the very least, try their free trial to explore the study materials risk-free.
This Nutrition Academy CNS program is also a great place to go for continuing education credits so that you may recertify with the IPTA for their CPT certification or if you plan to recertify with any other organization like the ISSA, NASM, NSCA, and more.
Let’s dive into the Study Guide now!
Study Guide – Chapter 1: What is a Nutrition Coach?
Introduction
Nutrition is central to human health, influencing energy, disease prevention, and overall well-being. Nutrition Coaches help clients make informed dietary choices by combining education, support, and personalized strategies. Unlike dietitians or doctors, they do not diagnose or prescribe treatment but focus on empowering behavior change.
Role of a Nutrition Coach
A Nutrition Coach bridges the gap between nutrition knowledge and everyday application. They translate general dietary advice into actionable steps for clients, helping them build lasting, healthy habits.
Key Functions:
- Education: Teach macronutrients, portion control, and meal planning.
- Support: Provide motivation and behavioral strategies.
- Accountability: Set and monitor goals with regular check-ins.
- Lifestyle Guidance: Encourage physical activity and balanced routines.
- Personalization: Adapt strategies to client preferences, culture, and lifestyle.
Responsibilities in Detail
- Education & Awareness – Simplify nutrition science into practical advice.
- Behavioral Support & Motivation – Use motivational interviewing, habit stacking, and self-monitoring to encourage consistency.
- Accountability & Goal Setting – Develop SMART goals (Specific, Measurable, Achievable, Relevant, Time-bound).
- Encouraging Physical Activity – Emphasize exercise as part of wellness (not as a trainer but as a lifestyle supporter).
- Personalized Support – Avoid one-size-fits-all advice; tailor recommendations based on unique needs.
What Nutrition Coaches Do Not Do
- Diagnose medical conditions.
- Prescribe Medical Nutrition Therapy (MNT).
- Recommend unproven supplements.
- Act outside their training (e.g., drug-nutrient interactions, therapeutic diets).
Key point: When issues exceed a coach’s expertise, referral to dietitians or medical professionals is essential.
Distinction from Other Professionals
Education
- Registered Dietitian (RD/RDN): Requires a degree, 1,200+ supervised hours, and a national exam. Licensed to provide clinical care.
- Nutrition Coach: Certification-based training (months to a year). Not licensed for clinical treatment.
- Nutritionist: Varies widely by location; sometimes regulated, often not.
Scope of Practice
- RDs: Can perform nutrition assessments, prescribe therapeutic diets, and interpret labs.
- Coaches: Provide general nutrition guidance and support habit change but cannot diagnose or prescribe.
Focus of Work
- RDs: Clinical problem-solving (e.g., designing diets for diabetes).
- Coaches: Practical support (meal prep strategies, overcoming cravings, creating sustainable routines).
Ethics and Professional Boundaries
Even when not legally regulated, coaches must follow ethical guidelines:
- Be transparent about qualifications.
- Maintain confidentiality.
- Obtain informed consent.
- Avoid misrepresenting themselves as medical providers.
Example: A client with high cholesterol –
- RD: Designs a diet targeting saturated fat reduction and fiber increase.
- Coach: Helps client apply the plan (swap butter for olive oil, eat oatmeal regularly, overcome dining-out challenges).
When to Refer Clients
Refer when clients:
- Show obsessive weight focus.
- Experience mental health struggles.
- Manage chronic conditions (e.g., kidney disease).
- Face pregnancy, breastfeeding, or gastrointestinal issues.
Referral does not mean ending the coaching relationship—it ensures the client receives safe, appropriate care.
Effectiveness of Nutrition Coaching
Research shows coaching is more effective than general diet advice because it addresses behavior change.
- Clients in structured coaching programs show improvements in weight, eating habits, and long-term adherence.
- Health coaching outperforms energy-restricted diets in weight loss success.
- Personalized plans reduce triglycerides, waist circumference, and body weight more effectively than generic guidelines.
Evidence-Based Practice (EBP)
Evidence-based coaching combines:
- Research evidence – Using peer-reviewed studies and dietary guidelines.
- Coach expertise – Applying personal training knowledge and practical skills.
- Client values/preferences – Considering cultural, financial, and lifestyle factors.
Example: Instead of promoting a trendy low-carb diet, an evidence-based coach evaluates research, the client’s goals, and feasibility, then tailors advice (e.g., partial Mediterranean diet adoption).
Training in Coaching Skills
Healthcare professionals increasingly incorporate coaching into practice. Training improves confidence in guiding patients toward healthy eating. Coaching is becoming a key tool in patient-centered care.
Collaboration in the Nutrition Field
Nutrition coaching works best when integrated into the healthcare continuum. Coaches complement professionals like dietitians, trainers, doctors, and psychologists.
Principles of collaboration:
- Holistic Care – Combine nutrition, behavior change, and exercise.
- Clear Referral Pathways – Know professional limits.
- Ethical Practice – Stay within scope and prioritize client safety.
Trainer Academy Nutrition Methodology
The methodology provides a framework for effective, ethical coaching:
- Evidence-Based Practice – Ground advice in research.
- Scope of Practice – Stay within legal/ethical boundaries.
- Client-Centered Coaching – Personalize, listen actively, and support empathy.
- Behavior Change Strategies – SMART goals, motivational interviewing, habit building.
- Nutritional Education & Empowerment – Teach clients to make their own informed choices.
- Holistic Approach – Address exercise, mental health, and lifestyle barriers.
- Ethical & Transparent Practices – Avoid false claims, protect privacy, maintain professionalism.
The Trainer Academy Difference
Trainer Academy emphasizes:
- Building trust and rapport.
- Supporting sustainable, long-term results.
- Elevating standards in nutrition coaching by integrating science with human behavior insights.
Conclusion
Nutrition Coaches are educators, motivators, and accountability partners. While they cannot diagnose or prescribe medical nutrition therapy, they play a vital role in helping people implement healthy behaviors. Their effectiveness comes from personalization, evidence-based practice, and collaboration with other health professionals.
By mastering behavioral strategies, ethical practice, and continuous learning, Nutrition Coaches make lasting impacts on client health and position themselves as essential members of the wellness field.
Study Guide – Chapter 2: The History of Food Culture
Introduction
Food is not just fuel—it reflects culture, identity, and community. Human food choices are shaped by sensory, biological, cultural, social, and economic forces. Over history, agriculture, trade, religion, and industrialization have driven the evolution of food cultures worldwide .
How Humans Choose Food
Sensory Perception
- Sight: Bright colors (red tomatoes, orange mangoes) signal freshness and nutrients; dull colors may suggest spoilage. Presentation and plating can enhance perceived quality.
- Smell: Aroma triggers appetite and cravings, often tied to memory and emotion (e.g., fresh bread, spices).
- Taste: Five basic tastes guide survival:
- Sweet = energy/calories
- Sour = fermentation/spoilage
- Salty = essential minerals
- Bitter = toxins (avoidance)
- Umami = protein/amino acids (satiety).
- Texture & Temperature: Crispness, creaminess, chewiness, and warmth/coolness affect enjoyment, speed of eating, and fullness .
Biological Needs
- Humans evolved to prefer calorie-dense foods (sugars, fats) due to survival pressures. Today, this drives cravings for processed foods.
- Specific hunger: Deficiencies (iron, salt) can trigger cravings for foods rich in those nutrients.
- Hunger hormones:
- Ghrelin = stimulates appetite.
- Leptin = signals satiety.
- Disruption (stress, leptin resistance, food cues) can override natural balance .
Psychological & Emotional Factors
- Emotional eating: Stress, sadness, boredom → craving comfort foods (ice cream, chips). Short-term relief, but linked to obesity and depression.
- Social influences: Eating patterns shaped by peers, family meals, holidays, and traditions (e.g., turkey at Thanksgiving, mooncakes at Mid-Autumn Festival).
- Preferences & aversions: Built from exposure, conditioning, associations, and change over time. Early exposure to cultural foods creates lifelong tastes .
Historical Food Evolution
Early Human Diets
- Hunter-gatherers ate wild fruits, nuts, vegetables, tubers, and hunted animals.
- Diets varied by region (coastal = seafood, inland = game/tubers).
- No processed foods; diets were high in fiber, moderate in fat, and low in sugar.
- Supported large brain development and evolutionary success.
- Modern “Paleo diet” attempts to replicate aspects of this pattern .
Agricultural Revolution (~10,000 years ago)
- Domestication of crops and animals allowed permanent settlements.
- Staple crops: wheat/barley (Middle East), rice (Asia), maize (Americas).
- Surpluses enabled trade routes (e.g., Silk Road, spice trade).
- Religion shaped food laws:
- Judaism (kosher)
- Islam (halal, no pork/alcohol)
- Hinduism (vegetarianism, beef restrictions).
- These practices reinforced cultural identity and sometimes improved health (e.g., avoiding spoilage-prone foods) .
Industrial Revolution (18th–19th centuries)
- Mechanization → increased crop yields, urban food supply.
- Food preservation (canning, pasteurization, refrigeration) extended storage and trade.
- Rise of processed foods: white flour, sugar, margarine, sodas, canned meals.
- Benefits: reduced famine, consistent supply.
- Drawbacks: increased obesity, heart disease, tooth decay .
Rise of the Western Diet
- Mid-20th century: diet high in processed meat, refined grains, sugar, fats.
- Low in fruits, vegetables, legumes, whole grains.
- Linked to obesity, type 2 diabetes, heart disease, cancers.
- Spread globally with economic growth and urbanization .
Cultural & Social Factors in Food
Traditions
- Foods reflect geography, climate, and heritage (sushi in Japan, curry in India, tacos in Mexico).
- Globalization spreads cuisines (pizza in China, curry in New York) but risks loss of local food knowledge .
Religion & Spirituality
- Dietary laws (kosher, halal, vegetarianism) and rituals (Ramadan fasting, Lent, Yom Kippur) influence eating patterns.
- Food often symbolizes prosperity, fertility, or unity .
Family & Community
- Shared meals reinforce social bonds.
- Family dinners linked to healthier diets in children.
- Community events and elders transmitting recipes preserve cultural identity.
- Social isolation can harm diet (reliance on processed foods) .
Economic Status
- Lower-income groups face “food deserts” (limited access to fresh foods).
- Healthier foods often cost more per calorie.
- Poorer populations rely on cheap, calorie-dense but nutrient-poor foods .
Media & Trends
- Advertising, celebrity endorsements, and now social media influencers shape choices.
- Viral foods (whipped coffee, avocado toast) spread globally.
- Social media drives both unhealthy diet fads and awareness of sustainable/plant-based eating.
- Food delivery apps increase convenience but also processed food intake .
The Future of Food Culture
Generational Shifts
- Younger generations emphasize fast, convenient foods; older ones value traditional cooking.
- Risk: cultural and health-promoting traditions (fermented foods, communal meals) may decline .
Nutrition Education & Coaching
- Traditional health professionals get little training in behavior change.
- Coaching methods (goal-setting, motivational interviewing) support long-term adherence better than strict diet prescriptions.
- Example: gradual reduction of sugary sodas vs. abrupt elimination .
Technology
- Apps, wearables, and AI tools track intake, activity, and biomarkers.
- Algorithms increasingly deliver personalized nutrition plans .
Sustainability
- Growing concern about climate and ethics:
- Plant-based diets reduce environmental impact.
- Fair trade, humane treatment, and regenerative agriculture gaining traction.
- Campaigns to reduce food waste (one-third of food wasted globally).
- Food choices now framed as both a health decision and an environmental responsibility .
Conclusion
The history of food culture shows a journey from hunter-gatherer diets to modern industrialized food systems, shaped by biology, culture, religion, trade, and technology. Today’s challenges include overconsumption of processed foods, loss of traditions, and sustainability concerns.
The future of nutrition lies in personalized, culturally sensitive, evidence-based coaching combined with sustainable practices that respect both human health and the planet.
Study Guide – Chapter 3: Defining Nutrition and Health
Introduction
Nutrition is fundamental for longevity, disease prevention, and well-being. It covers macronutrients (carbs, proteins, fats), micronutrients (vitamins, minerals), and extends to dietary patterns, food processing, and lifestyle. Poor diets are a leading modifiable risk factor for chronic diseases worldwide .
What is Physical Health?
Physical health is the body’s ability to function effectively and perform daily tasks.
Key Elements
- Optimal Functioning of Body Systems – All organs (cardiovascular, respiratory, digestive, musculoskeletal) working in harmony to sustain vitality.
- Absence of Disease – Aligns with WHO’s definition of complete well-being, not just lack of illness.
- Physical Fitness Components – Strength, endurance, flexibility, balance.
- Nutritional Adequacy – Proper intake of macro- and micronutrients supports energy, immunity, and recovery.
Differences Between Health and Fitness
- Health: Overall physical, mental, and social well-being; focus on disease prevention and balance.
- Fitness: Physical performance capacity; measurable attributes like endurance, strength, and body composition.
A person may be fit but unhealthy (e.g., an athlete with malnutrition) or healthy but unfit (no illness but poor conditioning). Optimal wellness combines both .
How Nutrition Supports Health & Fitness
Nutrition fuels performance, recovery, and disease prevention.
1. Energy Balance
- Calories in vs. calories out determines body weight and energy.
- Surplus → obesity, metabolic syndrome.
- Deficit → fatigue, muscle loss, nutrient deficiencies.
Maintaining balance sustains workouts and prevents disease .
2. Macronutrient Distribution
- Carbohydrates: Primary fuel, especially for brain & high-intensity exercise. Complex carbs > refined sugars.
- Proteins: Build/repair muscles, enzymes, hormones. Needed after exercise for recovery. Both plant and animal sources work. Excess red/processed meats increase CVD risk.
- Fats: Provide long-term energy, cell structure, hormones.
- Healthy: Unsaturated (olive oil, nuts, fish, omega-3s) → heart protective.
- Unhealthy: Trans fats & excess saturated fat → raise LDL, CVD risk .
3. Micronutrient Support
- Vitamins:
- B vitamins → energy metabolism, red blood cell formation.
- C & E → antioxidants against oxidative stress.
- Minerals:
- Calcium & magnesium → bone health, muscle/nerve function.
- Iron → oxygen transport, endurance.
- Zinc → immune defense, repair.
Deficiencies reduce performance and health .
4. Hydration
- Water = nutrient transport, temperature control, joint lubrication.
- Dehydration impairs performance; as little as 2% fluid loss reduces endurance.
- Replace fluids post-exercise (1.25–1.5 L per kg body weight lost). Include electrolytes for muscle/nerve function .
5. Role in Recovery
- Carbs: Restore glycogen after training.
- Protein (20–30 g): Repairs muscle and stimulates growth.
- Antioxidant/anti-inflammatory foods (berries, omega-3s): Reduce exercise-induced damage.
- Nutrient timing: Combining carbs + protein soon after training boosts adaptation .
6. Disease Prevention
- Diets low in added sugars, refined carbs, unhealthy fats prevent obesity, diabetes, CVD.
- High intake of fruits, vegetables, whole grains → lower chronic disease rates.
- Functional foods:
- Omega-3s → reduce triglycerides.
- Oats → lower LDL.
- Polyphenols (berries, green tea) → reduce inflammation .
Role of Nutrition in Longevity
Overall dietary patterns matter more than isolated nutrients. Research highlights:
Mediterranean Diet
- High in fruits, vegetables, whole grains, legumes, nuts, olive oil, seafood.
- Low red meat, sweets. Moderate wine.
- Benefits:
- ↓ Heart disease & stroke (24% lower CVD risk in meta-analyses).
- ↓ Type 2 diabetes & better blood sugar control.
- ↓ Cognitive decline and Alzheimer’s risk.
- Supported by the large PREDIMED trial .
DASH Diet (Dietary Approaches to Stop Hypertension)
- Emphasizes fruits, vegetables, whole grains, low-fat dairy, lean proteins.
- Low sodium (~1500–2300 mg/day), sweets, and red meat.
- Benefits:
- ↓ Blood pressure by ~5–6 mmHg (similar to medication).
- Improved cholesterol, insulin sensitivity.
- Lower diabetes risk .
Intermittent Fasting (IF) & Caloric Restriction (CR)
- IF: Alternating fasting/feeding periods (16:8, 5:2, etc.).
- Benefits: Weight loss, improved insulin sensitivity, reduced inflammation, autophagy.
- CR: Consistently lower calorie intake (20–40% less).
- Extends lifespan in animals, reduces age-related risk markers in humans.
- Downsides: Long-term CR may cause muscle loss, reduced bone density .
Nutrition and Disease Prevention
Cardiovascular Disease
- Healthy fats: Unsaturated fats & omega-3s improve cholesterol, reduce arrhythmias.
- Fiber: Lowers LDL, improves insulin sensitivity.
- Polyphenols: From fruits, veggies, olive oil → reduce oxidative stress, improve vascular function.
- Sodium & potassium balance: Lower sodium, higher potassium = better blood pressure.
- Alcohol: Possible mild benefit in moderation; excess harmful .
Diabetes
- Low GI foods: Beans, oats, whole grains → stable blood sugar, lower HbA1c.
- Fiber: Blunts glucose spikes.
- Healthy fats: MUFA/PUFA improve insulin sensitivity (e.g., olive oil, nuts).
- Lean proteins: Support satiety and control glucose response.
- Weight management: Losing 5–10% body weight improves control.
- Limit refined sugars & liquid calories .
Cognitive Health
- Leafy greens: Slow brain aging (up to 11 years younger in function).
- Berries: Flavonoids improve memory, reduce decline.
- Fatty fish & omega-3s (DHA): Support brain cell membranes, lower dementia risk.
- Nuts: Vitamin E and healthy fats improve cognition.
- Curcumin (turmeric): May reduce brain inflammation, amyloid plaques.
- MIND Diet (Mediterranean + DASH hybrid): 53% lower Alzheimer’s risk with high adherence .
Conclusion
Nutrition underpins every aspect of health—from energy and performance to disease prevention and longevity.
- Balanced diets rich in whole, plant-based foods reduce chronic disease risk.
- Modern approaches like IF and personalized nutrition show promise but should build on proven foundations like the Mediterranean and DASH diets.
- Future nutrition may be increasingly personalized (nutrigenomics, microbiome science), but general rules remain: eat a variety of nutrient-dense foods, stay hydrated, and limit processed foods.
Good nutrition is a lifelong investment in physical vitality, mental sharpness, and healthy aging.
Study Guide – Chapter 4: The Human Digestive System
Introduction
The digestive system is a complex network of organs, glands, and muscles that break down food, absorb nutrients, and remove waste. It performs six main functions:
- Ingestion – taking in food through the mouth.
- Propulsion – moving food along via swallowing and muscular contractions (peristalsis).
- Mechanical digestion – physical breakdown, such as chewing and churning in the stomach.
- Chemical digestion – enzymes, acids, and bile break nutrients into absorbable molecules.
- Absorption – nutrients and water pass into blood or lymph for distribution.
- Defecation – elimination of indigestible material as feces .
Muscles in Digestion
Digestion depends on several muscle groups:
- Smooth muscle lines most of the gastrointestinal tract. It contracts involuntarily to move food through peristalsis and mixes it with digestive juices in segmentation.
- Skeletal muscle is under voluntary control at the beginning and end of digestion. It powers chewing and swallowing in the mouth and pharynx, and also controls the external anal sphincter for defecation.
- Sphincter muscles regulate flow between digestive sections. The lower esophageal sphincter prevents reflux of stomach acid, and the pyloric sphincter controls how quickly chyme leaves the stomach and enters the small intestine .
Anatomy and Components
Mouth and Salivary Glands
Digestion begins in the mouth. Teeth and jaw muscles perform mastication, breaking food into smaller particles and mixing it with saliva. Saliva contains amylase, which begins breaking down starches into sugars, and lingual lipase, which begins lipid digestion, becoming more active in the stomach’s acidic environment. Saliva also provides lubrication and antimicrobial protection. Once food is chewed and moistened into a bolus, the tongue pushes it back to initiate swallowing. Reflex actions close off the nasal passage and airway to ensure the bolus enters the esophagus .
Esophagus
The esophagus is a muscular tube that connects the throat to the stomach. It does not digest food but transports the bolus through waves of peristalsis. Its lining secretes mucus to ease passage. At its lower end, the esophageal sphincter allows food to enter the stomach and closes afterward to prevent reflux. Weakness here can lead to heartburn or GERD .
Exclusive PTP CPT Offers |
||
|---|---|---|
Best Overall Cert | Best Online Cert | Best Study Materials |
Gold Standard Cert | A Good Option | Best CPT for you?  |
Stomach
The stomach acts as a temporary storage organ and initiates protein digestion. It churns food with gastric secretions to form chyme, a semi-liquid mixture. Gastric juice includes hydrochloric acid, which denatures proteins and kills microbes, and pepsinogen, which is activated to pepsin for protein breakdown. Gastric lipase adds some fat digestion. The stomach also produces intrinsic factor, required for vitamin B12 absorption later in the ileum. Protective mucus and bicarbonate shield the lining from acid. The pyloric sphincter regulates release into the small intestine, slowing emptying for fatty meals to allow efficient digestion .
Small Intestine
The small intestine is the main site of nutrient absorption and is divided into the duodenum, jejunum, and ileum.
- The duodenum receives chyme along with bile and pancreatic juice. Bile salts emulsify fats into smaller droplets, while pancreatic juice neutralizes stomach acid and supplies enzymes to digest carbohydrates, proteins, and fats.
- The jejunum is where most absorption occurs. Its folded lining with villi and microvilli vastly increases surface area. Sugars, amino acids, fatty acids, vitamins, and minerals are absorbed here, entering either the blood or lymph.
- The ileum continues absorption, particularly of vitamin B12 (bound to intrinsic factor) and bile salts for recycling. It also contains immune structures (Peyer’s patches) that help monitor gut microbes.
By the end of the ileum, about 90% of available nutrients and water have been absorbed .
Large Intestine
The large intestine, or colon, absorbs water and electrolytes and compacts waste. It is also home to the gut microbiota—trillions of bacteria that ferment undigested fiber to produce gases and short-chain fatty acids. These fatty acids, especially butyrate, provide energy to colon cells and support immune function. The microbiota also synthesize vitamin K and some B vitamins. The colon slowly propels material toward the rectum, consolidating it into feces for elimination .
Accessory Organs
- Liver produces bile for fat digestion and also processes absorbed nutrients.
- Gallbladder stores and releases bile when dietary fat is present. Gallstones can interfere with bile flow.
- Pancreas produces digestive enzymes (amylase, lipase, proteases) and bicarbonate, delivered into the duodenum. It also has endocrine functions such as insulin release.
Without bile and pancreatic enzymes, digestion of fats and proteins would be incomplete .
The Digestive Process Step by Step
- Ingestion and Chewing – food is broken down mechanically and mixed with saliva to begin carbohydrate and fat digestion.
- Swallowing – a reflex action pushes the bolus into the esophagus, where peristalsis carries it to the stomach.
- Stomach digestion – food is churned, proteins are broken down by pepsin, and chyme is formed.
- Small intestine – bile and pancreatic enzymes complete macronutrient breakdown; villi absorb most nutrients.
- Large intestine – water and electrolytes are reabsorbed, fiber is fermented by bacteria, and vitamins are synthesized.
- Defecation – waste is expelled after rectal stretch receptors trigger reflexes; voluntary relaxation of the external sphincter allows elimination .
Digestive Disorders
- GERD results from a weak esophageal sphincter allowing acid reflux, causing heartburn.
- Lactose intolerance occurs when lactase enzyme levels are low, leading to gas, bloating, and diarrhea after dairy intake. Common globally, it varies by genetics.
- Celiac disease is an autoimmune response to gluten, damaging the intestinal lining and impairing absorption. Strict gluten avoidance is required.
- IBS is a functional disorder with abdominal pain and altered bowel habits, often worsened by stress or certain foods.
- Constipation is linked to low fiber, dehydration, or inactivity and can often be corrected with diet and lifestyle adjustments.
- Non-celiac gluten sensitivity produces symptoms after gluten consumption without immune or intestinal damage .
Supporting Digestive Health
Digestive wellness depends on both diet and lifestyle. Key strategies include:
- Eating a fiber-rich diet with fruits, vegetables, legumes, and whole grains to regulate bowel movements and nourish gut microbes.
- Staying hydrated to ease stool passage and support nutrient transport.
- Eating mindfully and chewing thoroughly to improve digestion and reduce discomfort.
- Consuming smaller, more frequent meals to avoid reflux and bloating.
- Exercising regularly, which stimulates gut motility and supports microbiome diversity.
- Managing stress through practices like meditation or breathing exercises, since the gut-brain connection can influence conditions like IBS.
- Including probiotics from fermented foods and prebiotics from fibrous plants to maintain a healthy gut microbiome.
- Avoiding smoking and excessive alcohol, both of which impair digestive function.
- Identifying and addressing intolerances or sensitivities by adjusting food choices.
Conclusion
The digestive system transforms food into usable nutrients through both mechanical and chemical processes. Each organ has a unique role, and together they sustain energy, immunity, and growth. Accessory organs like the liver, gallbladder, and pancreas provide crucial support with bile and enzymes.
Understanding digestion helps coaches and health professionals guide clients toward better nutrition. By combining sound diet choices with habits like hydration, exercise, stress control, and microbiome support, individuals can optimize their digestive health, prevent common disorders, and enhance overall well-being.
Study Guide – Chapter 5: Energy Balance
Introduction
Energy balance and metabolism are at the core of nutrition and health. Energy balance is the relationship between calories consumed (intake) and calories burned (expenditure).
- Positive balance (intake > expenditure) → weight gain.
- Negative balance (intake < expenditure) → weight loss.
Metabolism includes all biochemical processes that convert food into usable energy, with anabolism (building) and catabolism (breaking down) working together to sustain life .
Components of Energy Balance
Energy Intake
Energy intake comes from macronutrients:
- Carbohydrates: 4 kcal per gram
- Proteins: 4 kcal per gram
- Fats: 9 kcal per gram
- Alcohol: 7 kcal per gram
Appetite is regulated by hormones, neural pathways, and behavior. Overeating leads to fat storage, while insufficient intake forces the body to draw on stored fat or muscle .
Energy Expenditure
Total Daily Energy Expenditure (TDEE) has three main parts:
- Basal Metabolic Rate (BMR): Energy needed for basic survival functions like breathing, circulation, and cell processes. About 60–70% of TDEE in sedentary people. Higher lean body mass raises BMR since muscle is metabolically active.
- Thermic Effect of Food (TEF): Calories burned digesting and absorbing food, about 5–10% of TDEE. Protein has the highest TEF, followed by carbs, and fat the lowest.
- Physical Activity: The most variable factor. Can account for 20–30% of expenditure in sedentary people, or 50%+ in very active people. Includes:
- Exercise Activity Thermogenesis (EAT): structured workouts.
- Non-Exercise Activity Thermogenesis (NEAT): everyday activities like walking, fidgeting, chores .
Calculating TDEE
TDEE = BMR × activity factor.
- Sedentary = BMR × 1.2
- Lightly active = BMR × 1.375
- Moderately active = BMR × 1.55
- Very active = BMR × 1.725
- Extra active = BMR × 1.9 .
Calorie Surplus and Deficit
- Surplus: Consistently eating more than expended → fat storage, weight gain. Useful for muscle growth with training, though some fat gain is inevitable.
- Deficit: Consuming fewer calories than burned → fat loss. A deficit of ~500 kcal/day usually produces ~1 lb (0.45 kg) weight loss per week. Too large a deficit risks muscle loss and metabolic slowdown .
Metabolic Energy Systems
The body uses three overlapping systems to produce ATP (the cell’s energy currency):
- ATP-Phosphocreatine (ATP-PC): Immediate, high-power energy from stored ATP and creatine phosphate. Fuels first seconds of intense activity.
- Glycolytic (Anaerobic Glycolysis): Breaks down glucose or glycogen for moderate-duration, high-intensity activity. Produces ATP quickly but limited.
- Oxidative (Aerobic): Slower, long-term ATP production from carbs, fats, and some protein using oxygen. Dominates during endurance activities .
Factors Affecting Energy Balance
- Sleep: Poor sleep lowers leptin (satiety) and raises ghrelin (hunger), increasing cravings. It also lowers metabolic rate and activity levels. Aim for 7–9 hours per night.
- Genetics & Physiology: Metabolic rate and fat storage tendencies vary by individual. Some naturally burn fewer calories at rest.
- Psychological/Environmental Factors: Stress and mood influence eating behavior. Chronic stress elevates cortisol, which raises appetite and promotes fat storage, especially abdominal .
Metabolic Adaptations
The body resists weight change through adaptive mechanisms (sometimes called set point theory).
- During calorie restriction, metabolism slows and hunger increases.
- During overfeeding, metabolism may rise slightly, but not enough to offset all extra intake.
This feedback makes both fat loss and long-term weight maintenance challenging .
Macronutrient Oxidation
- Carbohydrates: Burned first due to limited storage. High carb intake suppresses fat oxidation, favoring fat storage in surplus.
- Fats: Easily stored; oxidized more when carbs are low. High-fat diets with high calories still lead to fat gain.
- Protein: Rarely stored; primarily used for tissue repair. Excess is burned or converted. High protein boosts metabolism and reduces hunger, helping with fat loss .
Metabolic Flexibility: Ability to switch between carbs and fats as fuel. Obesity often reduces this flexibility, impairing fat burning and contributing to insulin resistance .
Hormonal Regulation
Key hormones controlling metabolism and appetite:
- Insulin: Moves glucose into cells; high levels encourage fat storage.
- Leptin: Made by fat cells; normally reduces hunger, but leptin resistance can blunt this effect.
- Ghrelin: Stimulates hunger; rises before meals, falls after. Increased with dieting or poor sleep.
- Thyroid hormones (T3, T4): Regulate metabolism; imbalances affect weight gain/loss.
- Catecholamines (epinephrine, norepinephrine): Increase fat burning during activity.
- Cortisol: Stress hormone; chronic elevation promotes fat gain.
- Sex hormones: Testosterone builds muscle and supports leanness; estrogen influences fat storage and shifts with menopause .
Impact of Diet Composition
- High-fat diets: Easy to overeat since fat is calorie-dense and has low thermic effect. Excess fat is easily stored, though unsaturated fats are healthier than saturated/trans.
- Carbohydrate quality: Refined carbs spike blood sugar and increase hunger. Whole, fiber-rich carbs digest slowly and improve satiety. Traditional high-carb diets rich in whole foods (like in Blue Zones) support healthy weight.
- Protein intake: Most filling macronutrient. Requires more energy to digest, preserves muscle during fat loss, and supports a higher metabolism. Around 25–30% of daily calories or 1.2–1.6 g/kg body weight is optimal .
Strategies to Maintain Energy Balance
- Move more: Combine cardio for calorie burn and strength training to preserve muscle. Add lifestyle activity (walking, stairs, chores).
- Eat mindfully: Chew thoroughly, avoid distractions, and control portions. Protein and fiber-rich meals enhance fullness.
- Supportive food environment: Keep healthy foods accessible and limit junk food. Cooking at home helps control calories.
- Protect metabolism: Avoid extreme calorie cuts. Use moderate deficits, eat adequate protein, and train with resistance.
- Sleep and stress management: Rest regulates hunger hormones, while stress reduction prevents overeating. Social support and tracking progress help maintain habits .
Beyond “Calories In, Calories Out”
While calorie balance determines weight change, newer models add nuance:
- Energy Balance Model (EBM): Ultra-processed foods disrupt appetite signals and increase intake unconsciously.
- Carbohydrate-Insulin Model (CIM): High refined carb intake raises insulin, increasing fat storage and hunger.
- Critiques of Classic Model: Simply telling people to “eat less, move more” ignores metabolic and hormonal adaptations.
- Food Environment: Portion sizes, availability of junk food, and sedentary lifestyles promote overeating.
- Energy Availability: Especially for athletes, low energy availability (even with stable weight) harms hormones, performance, and health .
Conclusion
Energy balance is shaped by calorie intake, expenditure, hormones, sleep, stress, and environment.
- Calories matter most for weight change, but macronutrient composition and lifestyle influence satiety, metabolism, and fat storage.
- Practical strategies include exercise, mindful eating, portion control, stress management, and sleep quality.
- For long-term success, the focus should be on sustainable balance, not crash diets or rigid calorie counting.
Understanding energy balance equips professionals to design nutrition plans that support weight management, disease prevention, and optimal health.
Study Guide – Chapter 6: Carbohydrates
Introduction
Carbohydrates are the body’s primary energy source, supplying fuel for the brain, muscles, and vital organs. They come in different forms—sugars, starches, and fiber—and play roles not only in energy metabolism but also in digestive health and disease prevention. Understanding carbohydrate structure, digestion, and function is essential for nutrition coaching .
Types of Carbohydrates
Simple Carbohydrates
- Monosaccharides – single sugar units. Examples:
- Glucose: main energy source for cells.
- Fructose: found in fruits and honey.
- Galactose: part of lactose in milk.
- Disaccharides – two sugar units:
- Sucrose (glucose + fructose).
- Lactose (glucose + galactose).
- Maltose (two glucose units).
Simple carbs digest quickly, giving rapid energy but often causing blood sugar spikes .
Complex Carbohydrates
- Oligosaccharides: 3–10 sugar units, found in beans, onions, and whole grains. Often act as prebiotics to support gut bacteria.
- Polysaccharides: long chains like starch (plants) and glycogen (storage form in animals).
- Fiber: indigestible plant carbohydrates.
- Soluble fiber dissolves in water, forming gels that slow digestion and lower cholesterol.
- Insoluble fiber adds bulk to stool, preventing constipation .
Digestion and Absorption
Carbohydrate digestion begins in the mouth with salivary amylase breaking starch into maltose.
- In the small intestine, pancreatic amylase continues starch breakdown, and brush-border enzymes split disaccharides into monosaccharides.
- Glucose and galactose are absorbed actively, while fructose is absorbed more slowly via facilitated diffusion.
- Once in the bloodstream, glucose supplies energy or is stored as glycogen in the liver and muscles .
Functions of Carbohydrates
- Energy Production – Glucose fuels the brain and high-intensity exercise. One gram provides ~4 kcal.
- Protein Sparing – Adequate carbs prevent the breakdown of protein for energy.
- Fat Metabolism – Carbs are needed to fully metabolize fat; low-carb intake can lead to ketone buildup.
- Digestive Health – Fiber promotes regularity, feeds beneficial gut bacteria, and lowers risk of colon disease.
- Chronic Disease Prevention – Fiber-rich carbs reduce risk of type 2 diabetes, heart disease, and obesity .
Blood Sugar Regulation
The body maintains blood glucose through hormones:
- Insulin lowers blood sugar by helping cells absorb glucose for use or storage.
- Glucagon raises blood sugar by stimulating glycogen breakdown.
- Balanced blood sugar is critical for energy stability, athletic performance, and long-term health .
Carbohydrates and Health
Weight Management
Excess refined carbs contribute to weight gain due to low satiety and high calorie density. Fiber-rich carbs promote fullness and reduce overall intake. Diet quality is more important than carb quantity alone.
Diabetes
Diets high in refined carbohydrates raise blood glucose and insulin demand, worsening insulin resistance. Choosing low-glycemic, fiber-rich carbs supports better blood sugar control.
Cardiovascular Health
Soluble fiber lowers LDL cholesterol. Whole grains and legumes are associated with reduced heart disease risk.
Gut Health
Prebiotic fibers fuel beneficial bacteria, producing short-chain fatty acids that support immune function and colon health .
Carbohydrate Recommendations
- Dietary Guidelines: 45–65% of daily calories from carbohydrates.
- Fiber Intake: 25 g/day for women, 38 g/day for men. Most people fall short of this.
- Added Sugars: Limit to <10% of total daily calories (ideally <5% for optimal health).
- Athletic Performance: Carbs are essential for endurance sports. Athletes often require higher intake to maintain glycogen stores .
Practical Coaching Applications
- Encourage clients to choose whole, minimally processed carbs such as fruits, vegetables, legumes, and whole grains.
- Emphasize fiber intake for digestive and metabolic health.
- Reduce intake of refined sugars and sugary drinks, which provide energy without nutrients.
- Teach timing strategies: higher carb intake before and after workouts aids performance and recovery.
- Use personalization: some clients thrive with moderate to high-carb diets, while others benefit from lower-carb approaches depending on health and activity .
Conclusion
Carbohydrates are not “bad”; they are a vital macronutrient providing energy, supporting performance, and promoting long-term health. The key lies in carbohydrate quality—choosing whole, fiber-rich sources over refined sugars. For coaches, guiding clients toward balanced carb intake tailored to their lifestyle and goals is central to effective nutrition planning.
Study Guide – Chapter 7: Lipids
Introduction
Lipids—fats, oils, phospholipids, and sterols—are essential nutrients that provide energy, form cell structures, and regulate hormones. They are calorie-dense (9 kcal per gram), making them the body’s most concentrated energy source. While often seen negatively, lipids are crucial for health when consumed in the right types and amounts.
Types of Lipids
Triglycerides
- Make up ~95% of dietary fat.
- Structure: glycerol backbone + three fatty acids.
- Functions: energy storage, insulation, protection of organs, and fat-soluble vitamin transport (A, D, E, K).
Fatty Acids
- Classified by saturation:
- Saturated fatty acids: no double bonds; solid at room temp (butter, lard). Excess linked to heart disease.
- Monounsaturated fatty acids (MUFA): one double bond; found in olive oil, nuts, avocado. Improve cholesterol.
- Polyunsaturated fatty acids (PUFA): multiple double bonds; include omega-3s and omega-6s.
- Omega-3s (EPA, DHA, ALA): reduce inflammation, support heart and brain health. Found in fish, flax, walnuts.
- Omega-6s: found in vegetable oils; necessary but often consumed in excess. Balance with omega-3s is key.
- Trans fats: artificially hydrogenated oils; increase LDL, lower HDL, and strongly linked to cardiovascular disease.
Phospholipids
- Structure: glycerol + 2 fatty acids + phosphate group.
- Function: form cell membranes, aid fat transport in blood (as lipoproteins). Example: lecithin.
Sterols
- Cholesterol is the main sterol.
- Functions: forms cell membranes, makes bile, vitamin D, and steroid hormones.
- Found in animal products, but the body also synthesizes it. Excess can raise cardiovascular risk.
Digestion and Absorption
- Mouth & Stomach: Minimal fat digestion; gastric lipase begins breakdown.
- Small Intestine: Major site. Bile salts from the liver emulsify fats into micelles. Pancreatic lipase breaks triglycerides into fatty acids and monoglycerides.
- Absorption: Products are absorbed into intestinal cells, reassembled into triglycerides, and packaged into chylomicrons for transport via the lymph and blood.
- Transport: Lipoproteins carry lipids:
- Chylomicrons: transport dietary fat.
- VLDL: deliver triglycerides from liver to tissues.
- LDL (“bad cholesterol”): deliver cholesterol to cells; high levels increase CVD risk.
- HDL (“good cholesterol”): remove excess cholesterol, transporting it to the liver for disposal.
Functions of Lipids
- Energy: Long-term fuel; crucial during rest and low-intensity exercise.
- Structural: Phospholipids and cholesterol maintain cell membrane integrity.
- Hormonal: Steroid hormones (testosterone, estrogen, cortisol) are derived from cholesterol.
- Nutrient Transport: Essential for absorbing fat-soluble vitamins.
- Insulation & Protection: Cushion organs and preserve body heat.
Lipids and Health
Cardiovascular Disease (CVD)
- Diets high in saturated and trans fats raise LDL cholesterol, leading to atherosclerosis.
- Replacing these with MUFAs and PUFAs reduces risk.
- Omega-3s lower triglycerides, reduce blood clotting, and improve heart rhythm.
Obesity
- Fats are calorie-dense and easy to overconsume. Moderation is essential for weight management.
Inflammation
- Balance of omega-3 to omega-6 intake affects inflammatory pathways. Western diets often favor omega-6, contributing to chronic inflammation.
Cancer
- Excess fat intake, especially saturated and trans fats, may promote certain cancers. Protective effects come from omega-3s and plant-based fats.
Lipid Recommendations
- AMDR (Acceptable Macronutrient Distribution Range): 20–35% of total calories from fat.
- Saturated fat: <10% of calories (ideally <7% for heart health).
- Trans fat: avoid completely.
- Omega-3 intake: ~250–500 mg/day of EPA + DHA recommended for adults.
- Cholesterol: no longer has a strict upper limit, but moderation is advised.
Practical Coaching Applications
- Encourage clients to replace butter, lard, and processed snacks with olive oil, nuts, seeds, and fatty fish.
- Stress the importance of reading food labels to avoid hidden trans fats.
- For athletes, highlight fat as a critical energy source for endurance. Balance intake with carbs and protein to optimize performance.
- Teach portion control—since fats are calorie-dense, even healthy fats can contribute to excess calories if not managed.
Conclusion
Lipids are often misunderstood but are essential for energy, health, and performance. The focus should not be on avoiding fat altogether, but on choosing the right types: limit saturated fats, eliminate trans fats, and prioritize unsaturated fats, especially omega-3s. Proper lipid balance supports cardiovascular health, hormone production, nutrient absorption, and long-term wellness.
Study Guide – Chapter 8: Supplements
Introduction
Supplements can help fill nutrient gaps, enhance performance, and support specific health conditions. However, they should supplement, not replace a balanced diet. Nutrition Coaches must know their types, benefits, risks, and regulations .
Classification of Supplements
According to DSHEA (U.S. law), dietary supplements are orally consumed products containing one or more dietary ingredients such as:
- Vitamins & minerals – essential micronutrients like vitamin D and iron.
- Proteins & amino acids – whey protein, BCAAs for muscle repair.
- Herbal extracts – ginseng, echinacea for therapeutic use.
- Probiotics & prebiotics – support gut health.
- Ergogenic aids – creatine, beta-alanine, caffeine .
Roles in Nutrition
- Addressing Deficiencies: Pregnant women (folic acid, iron), older adults (calcium, vitamin D), vegans (B12, omega-3s), and those with restricted diets often benefit .
- Athletic Performance: Evidence supports creatine, beta-alanine, caffeine, and BCAAs.
- Chronic Disease: Supplements like omega-3s, vitamin D, and probiotics show promise in reducing risks .
Safety and Regulation
Risks
- Overconsumption: High doses can cause toxicity (e.g., fat-soluble vitamins).
- Drug Interactions: Example: St. John’s Wort reduces effectiveness of some medications.
- Adulteration: Some weight loss or muscle-building products contain hidden drugs .
Regulation
- In the U.S., supplements are regulated as foods, not drugs. No FDA pre-market approval is required—safety oversight is mostly post-market.
- Other regions (EU, Canada, Australia) require stricter testing before sale .
- Consumers should choose third-party tested products (USP, NSF, Informed Sport).
Practical Guidelines
- Assess Need: Review diet logs, lifestyle, and medical conditions.
- Choose Quality: Third-party certifications, transparent labeling, good manufacturing practices.
- Educate Clients:
- Food-first approach.
- Proper dosages and timing.
- Avoid exaggerated claims.
- Evaluate Continuously: Monitor effectiveness, safety, and legality for athletes .
Ergogenic Aids
Creatine: Best for short, high-intensity activity. Improves ATP regeneration, strength, and lean mass. Typical protocol: 20 g/day for 5–7 days, then 3–5 g/day. Safe long term .
Caffeine: Boosts endurance, reduces fatigue, and improves focus. Effective at 3–6 mg/kg ~1 hour before exercise. Too much causes jitters, anxiety, and sleep disruption .
Beta-Alanine: Raises muscle carnosine, buffering acidity. Best for high-intensity efforts lasting 1–10 minutes. Dose: 4–6 g/day for weeks. Side effect: harmless tingling .
BCAAs: Leucine, isoleucine, valine. May reduce soreness and support protein synthesis, but less effective if overall protein intake is adequate. Typical: 5–10 g before/during training .
Betaine: Found in beets. May improve body composition and strength; dose ~2.5 g/day. Safe and well-tolerated .
Citrulline Malate: Boosts nitric oxide, improves blood flow and endurance. Effective at 6–8 g pre-workout. Safe and generally well-tolerated .
Protein Supplements
Protein powders (whey, casein, soy, pea, rice) are popular for recovery and growth.
- Whey: Fast-digesting, high leucine, ideal post-workout.
- Casein: Slow-digesting, useful before sleep.
- Plant-based: Effective if combined/blended.
- Recommended Intake: 1.6–2.2 g/kg/day for athletes. Powders are a convenient tool, not essential if diet is sufficient .
Weight Loss Supplements
- Caffeine & Stimulants: Slightly increase metabolism and calorie burn.
- Green Tea Extract (EGCG): Small added fat loss when combined with caffeine.
- CLA: Very modest fat reduction, inconsistent results.
- Fiber (glucomannan, psyllium): Increases fullness, supports appetite control.
- Garcinia Cambogia, Raspberry Ketones, etc.: Weak or no evidence.
⚠️ Many weight loss products are adulterated or unsafe. Sustainable fat loss comes from diet and exercise .
Health Supplements
- Fish Oil (Omega-3s): Lowers triglycerides, supports heart/brain health. Dose: 250–500 mg EPA + DHA/day; higher for clinical needs .
- Multivitamins: Insurance for those with poor diets; not a replacement for whole foods.
- Vitamin D: Crucial for bone and immune health. Many are deficient. Typical dose: 1000–2000 IU/day, adjusted for baseline levels .
- Magnesium: Involved in >300 reactions. Supports muscle/nerve function, reduces inflammation, may improve sleep and anxiety. Dose: 310–420 mg/day; citrate/glycinate preferred .
Banned Substances
Athletes must avoid prohibited compounds (steroids, SARMs, HGH, EPO, amphetamines, clenbuterol, diuretics).
- Risks include organ damage, hormone disruption, psychiatric issues, and legal/ethical consequences.
- Some supplements are unknowingly contaminated—athletes should only use products with NSF/Informed Sport certifications .
Conclusion
Supplements can:
- Fill nutrient gaps (e.g., vitamin D, iron, B12).
- Enhance performance (creatine, caffeine, beta-alanine).
- Support health (omega-3s, probiotics, magnesium).
But they also carry risks: contamination, interactions, or false claims. Coaches must emphasize a food-first approach, evidence-based choices, and safety. The guiding principle: use only what’s necessary, safe, and supported by research.
Study Guide – Chapter 9: Hydration
Introduction
Water makes up about 50–60% of body weight and is vital for nearly every physiological process. It acts as a building material, solvent, transporter, waste remover, and temperature regulator. Because the body cannot store excess water, hydration must be continuously maintained. Even mild dehydration (1–2% body weight) can impair cognition, mood, and exercise performance .
Body Water Balance
Water is distributed between intracellular fluid (ICF, ~⅔ of total) and extracellular fluid (ECF, ~⅓). Sodium dominates the ECF, while potassium dominates the ICF. Water shifts via osmosis to balance concentrations.
Key regulatory systems:
- ADH (antidiuretic hormone): conserves water by reducing urine output.
- Renin-angiotensin-aldosterone system: increases thirst and sodium reabsorption, with water following.
Even a 1% body water loss triggers these mechanisms, while larger losses impair organ function .
Functions of Water
- Thermoregulation: Sweating and skin blood flow prevent overheating.
- Nutrient Transport: Plasma is 90% water, carrying oxygen, glucose, and nutrients.
- Waste Removal: Kidneys require water to excrete urea and toxins; dehydration increases kidney stone risk.
- Lubrication & Cushioning: Synovial fluid supports joints; moisture protects tissues.
- Cognitive Function: Even mild dehydration reduces concentration, mood stability, and memory .
Role of Sodium (Salt)
Sodium is the main electrolyte in the ECF and critical for:
- Fluid balance: “Where sodium goes, water follows.”
- Blood pressure regulation: Sodium levels influence vascular volume.
- Nerve & muscle function: Sodium influx generates action potentials for nerve signals and contractions.
- Nutrient absorption: Facilitates glucose and amino acid uptake in the gut .
Electrolyte Imbalances
- Hyponatremia: Low blood sodium from overhydration or heavy sweating without replacement. Leads to swelling of cells, confusion, seizures, and even death.
- Hypernatremia: Excess sodium concentration from dehydration. Causes cellular shrinkage, confusion, and muscle twitching.
Both stress the importance of balancing water + electrolyte intake .
Daily Water Intake
Guidelines (Institute of Medicine):
- Men: ~3.7 L/day (15–16 cups).
- Women: ~2.7 L/day (11–12 cups).
Intake varies with activity, climate, and body size .
Hydration states:
- Euhydration = normal levels.
- Hypohydration = low body water.
- Hyperhydration = excess water.
- Underhydration = inadequate intake before deficits become obvious .
Hydration and Exercise
During exercise, metabolic heat is dissipated through sweating. Sweat rates vary (0.3–2.4 L/hour). Losses above 2% of body mass impair:
- Thermoregulation (rising core temp).
- Cardiovascular function (higher HR, reduced blood flow).
- Endurance, strength, and cognition.
Sweat must evaporate to cool the body; high humidity limits evaporation, raising heat illness risk .
Cognitive, Muscular, and Metabolic Effects
- Cognition: Dehydration impairs attention, memory, and mood. Elderly and children are especially vulnerable.
- Muscles: Reduced nutrient/oxygen delivery accelerates glycogen depletion, fatigue, and oxidative stress.
- Recovery: Fluids (with sodium and carbs) support faster glycogen resynthesis and waste removal .
Hydration Strategies for Athletes
- Pre-Exercise: 500–600 mL 2–3 hrs before, plus 200–300 mL 10–20 min before. Urine color is a quick hydration check.
- During Exercise: 200–300 mL every 10–20 minutes (~0.6–1.2 L/hour). For >60–90 min, use sports drinks with carbs + sodium. Goal: limit body mass loss to <2%.
- Post-Exercise: Replace ~125–150% of fluid lost (1.25–1.5 L per kg of weight lost). Include sodium and protein for better retention and recovery (e.g., chocolate milk) .
Special Considerations
- Extreme environments: Heat/humidity increase sweat loss; cold reduces thirst but still risks dehydration. Hyperhydration strategies or ice slurries may help.
- Individual variability: Sweat testing helps personalize hydration plans based on sweat rate and sodium content.
Hydration and Long-Term Health
- Urinary health: Extra fluid reduces risk of UTIs and kidney stones.
- Digestive health: Prevents constipation by softening stool.
- Metabolic health: Better hydration linked to healthier weight and blood sugar regulation.
- Chronic disease risk: Underhydration associated with obesity, heart disease, insulin resistance, and premature mortality .
Conclusion
Hydration is critical for daily function, performance, and long-term health. Both water and electrolytes must be consumed in balance. For athletes, structured hydration before, during, and after exercise preserves endurance, strength, cognition, and recovery. Beyond sports, consistent hydration lowers risks of kidney stones, constipation, and chronic disease.
Key takeaway: Staying well-hydrated is one of the simplest, most effective ways to optimize performance and health.
Study Guide – Chapter 10: Alcohol and Nutrition
Introduction
Alcohol has been part of human culture for thousands of years. While moderate use has sometimes been linked to heart benefits, excessive or chronic drinking harms nutrition and health. Alcohol contributes calories but few nutrients, disrupts metabolism, and increases the risk of nutrient deficiencies and chronic disease .
Alcohol as a Macronutrient
- Energy value: 7 kcal per gram (more than carbs/protein, less than fat).
- Empty calories: No vitamins, minerals, or essential nutrients.
- Heat loss: Not all alcohol calories are stored; some are lost as heat.
- Metabolic disruption: Liver prioritizes alcohol breakdown, temporarily halting fat burning. This promotes fatty liver disease .
Alcohol and Calorie/Nutrient Intake
- Substitution effect: Heavy drinkers (4–5 drinks/day) often replace nutrient-rich food with alcohol calories, leading to protein, fat, and carb deficiencies.
- Overeating: Alcohol lowers self-control and boosts appetite, encouraging junk food consumption.
- Malnutrition risk: Even with high calorie intake, diet quality declines, resulting in nutrient deficiencies over time .
Micronutrient Deficiencies from Alcohol
Chronic alcohol intake is strongly linked to:
- Thiamine (B1): Deficiency may cause Wernicke–Korsakoff syndrome, affecting memory and coordination.
- Folate (B9) and other B vitamins: Leads to anemia, nerve issues, and higher heart disease risk.
- Fat-soluble vitamins (A, D, E, K): Interferes with storage and activation; causes vision problems, bone loss, weak immunity, and clotting issues.
- Minerals (magnesium, zinc, iron): Poor absorption or losses lead to cramps, poor healing, immunity issues, or abnormal iron levels .
Alcohol, Body Composition, and Metabolic Health
Alcohol’s effects are complex:
- “Wasted” calories: Up to 30% of alcohol’s calories are burned as heat.
- Muscle loss: Heavy drinking reduces protein synthesis and accelerates breakdown (alcoholic sarcopenia).
- Fat distribution: Promotes visceral fat around organs, raising risk for metabolic syndrome, diabetes, and CVD—even if BMI remains normal .
Liver and Nutrient Metabolism
The liver is central to nutrient processing, but alcohol damages its function:
- Vitamin storage & activation: Poor storage of A, B12, folate, and impaired conversion (e.g., carotene → vitamin A).
- Macronutrient metabolism: Excess NADH from alcohol disrupts carb, fat, and protein metabolism, leading to fatty liver, low blood sugar, insulin resistance, and toxin buildup.
- Oxidative stress: Free radical damage worsens liver injury while depleting antioxidants (vitamins C, E, selenium) .
Protein–Energy Malnutrition (PEM)
- Heavy drinkers may get >50% of calories from alcohol, displacing food.
- Leads to weight loss, muscle wasting (marasmus-like), or swelling from protein deficiency (kwashiorkor-like).
- Combined with gut damage and liver dysfunction, PEM causes weakness, infections, poor wound healing, and fluid retention .
Alcohol’s Effect on Diet and Lifestyle
- Food preferences: Promotes cravings for salty, sugary, high-fat snacks.
- Low nutrient-dense foods: Heavy drinkers eat fewer fruits, vegetables, and whole grains.
- Erratic meal timing: Skipping meals, late-night binges, or “saving calories” for alcohol disrupt metabolism.
- Social/economic factors: Alcohol spending and isolation reduce ability to buy or prepare healthy food .
Bidirectional Relationship: Diet and Alcohol
Diet also influences alcohol behavior:
- High-carb diets: May reduce cravings by boosting serotonin.
- High-protein/low-carb diets: May increase cravings by enhancing dopamine signals.
- Sweet cravings: People with alcohol use disorder often crave sugar, since both trigger brain reward pathways.
- Gut–brain axis: Fiber-rich diets improve mood and reduce cravings; sugar-heavy diets may worsen them .
Guidelines for Alcohol and Nutrition
- Moderation: ≤1 drink/day for women, ≤2 for men. Binge drinking is harmful even if rare. No need to start drinking for health.
- Avoid completely: Pregnant women, minors, people with liver/pancreatic disease, high blood pressure, ulcers, or drug interactions.
- Nutrient support: Regular drinkers often need extra B vitamins (thiamine, folate, B12), vitamin D, magnesium, and zinc.
- Balanced diet: Eat regular meals with protein, healthy fats, and fiber; never drink on an empty stomach.
- Hydration: Alternate alcohol with water to reduce dehydration and hangover risk .
Coaching Strategies
- Education: Clarify alcohol’s calorie load (cocktails can equal meal calories).
- Goal alignment: Link alcohol reduction to client goals (weight loss, muscle gain, better recovery).
- Behavioral support: Identify triggers and encourage alternatives (exercise, tea, hobbies). Track drinks to build awareness.
- Referral: If signs of alcohol use disorder (AUD) appear, refer to medical/psychological support or programs like AA/SMART Recovery .
Moderate vs. Heavy Drinking
- Moderate: May not harm nutrient status in balanced diets, though risks still exist (e.g., folate-related cancer risk).
- Heavy: Severe disruptions in macro- and micronutrient balance, muscle loss, liver failure, and long-term malnutrition.
- Key point: Moderate drinking is a ceiling, not a recommendation. Abstinence is safest nutritionally .
Conclusion
Alcohol provides calories but undermines nutrition by displacing food, impairing absorption, and damaging the liver. Moderate drinking may fit within a healthy diet, but it carries risks. Coaches should help clients:
- Prioritize food-first nutrition.
- Stay within low-risk drinking limits.
- Monitor nutrient deficiencies.
- Refer out when dependence signs appear.
Ultimately, alcohol and nutrition are deeply linked—improving diet can help reduce drinking, and addressing alcohol use supports better nutrition.
Study Guide – Chapter 11: The Role of Evidence-Based Practice
Introduction
Nutrition coaches face a flood of diet trends and health claims. To separate fact from fad, they rely on evidence-based practice (EBP): combining the best research, professional expertise, and the client’s unique needs. This ensures advice is both scientifically credible and personalized .
What is Evidence-Based Practice?
EBP in nutrition is built on three pillars:
- Best Evidence – Use high-quality, up-to-date research and official guidelines.
- Coach Expertise – Apply professional judgment and experience to interpret studies.
- Client Values & Preferences – Adapt findings to fit cultural background, food preferences, and lifestyle .
Why Research Quality Matters
Not all studies are equally reliable. Coaches should always ask:
- Is this a good study? (internal validity – strong design, randomization, control groups).
- Is it relevant to my client? (external validity – does it apply to real-world settings?).
High-quality, relevant evidence carries the most weight, while sensational headlines from weak studies should be treated with skepticism .
Steps of the Evidence-Based Process (5 A’s)
- Ask – Frame a clear question (use PICO: Population, Intervention, Comparison, Outcome).
- Acquire – Search credible sources (PubMed, Cochrane Library, USDA, EAL).
- Appraise – Critically evaluate evidence for reliability, study design, sample size, and biases.
- Apply – Combine findings with expertise and client preferences for realistic recommendations.
- Assess – Monitor client outcomes and adjust strategies as needed .
Types of Evidence (Hierarchy)
- Top tier: Clinical guidelines, systematic reviews, meta-analyses – summarize many studies for strong conclusions.
- Randomized Controlled Trials (RCTs): Gold standard for cause-effect testing.
- Observational Studies: Useful for long-term diet patterns, but only show associations.
- Expert Opinion: Helpful when research is limited, but influenced by bias.
- Anecdotes & Testimonials: Lowest tier, not reliable evidence .
Key principle: Look for weight of evidence. Multiple studies pointing in the same direction are more trustworthy than a single small trial.
Bias and Limitations in Research
Common issues in nutrition research:
- Selection bias: Participants don’t represent general population.
- Recall/self-report bias: Diets reported inaccurately by participants.
- Confounding variables: Other lifestyle factors (exercise, income) may explain results.
- Small or short studies: May not capture long-term effects.
- Funding conflicts: Industry sponsorship may skew findings .
Being aware of bias prevents overreacting to every flashy headline. Coaches should weigh results carefully and consider the totality of evidence.
Embracing Uncertainty and Staying Current
Nutrition science evolves—guidelines change as new data emerges (e.g., from low-fat to focusing on fat quality). Coaches should:
- Keep up with major updates (Dietary Guidelines, consensus reports).
- Look for consistency across studies before drawing conclusions.
- Be transparent with clients about the strength of evidence.
- Admit when evidence is limited and adjust recommendations as science advances .
Applying EBP with Clients
Practical application requires flexibility:
- Tailor to the individual: Even if keto shows short-term weight loss benefits, it may not suit a client who enjoys fruits and grains. A moderate lower-carb approach may be better.
- Consider safety: Intermittent fasting may benefit some, but could worsen disordered eating in others.
- Merge client ideas with evidence: If a client wants to try a trendy supplement with weak evidence, acknowledge the limits, monitor effects, but emphasize proven strategies like increasing vegetables.
Shared decision-making is essential—clients are more likely to follow a plan they helped design .
Tools and Resources for Coaches
Key resources that save time and provide reliable evidence:
- Dietary Guidelines for Americans – Updated every 5 years, free online.
- Evidence Analysis Library (EAL): Evidence summaries on nutrition questions.
- Cochrane Library: Rigorous systematic reviews.
- PubMed & Google Scholar: Search databases for research.
- Professional Consensus Statements: From organizations like the ADA or WHO.
- Appraisal Tools: CASP checklists, NUQUEST (nutrition-specific quality tools).
- Continuing Education & Networks: Webinars, professional associations, and forums focused on evidence-based practice .
Conclusion
Evidence-based practice is not a rigid formula but a mindset and process. It requires continuously asking:
- What does the science say?
- How does it apply to this client?
By integrating research with expertise and client values, coaches build credibility, trust, and effectiveness. Nutrition coaching becomes both a science (grounded in evidence) and an art (personalized communication and application).
Key takeaway: EBP empowers coaches to provide accurate, ethical, and client-centered nutrition advice in a constantly changing scientific landscape.
Study Guide – Chapter 12: How to Read Food Labels
Introduction
Food labels provide essential information about ingredients, nutrients, allergens, and serving sizes. Understanding them helps consumers make healthier choices. However, many people misinterpret labels, leading to overeating or reliance on misleading claims. This chapter explains the main label components, common pitfalls, and strategies to build label literacy .
Key Components of Food Labels
Nutrition Facts Panel
- Serving size & servings per container: Always check first. Eating multiple servings means doubling or tripling the listed values.
- Calories: Provided per serving. Remember that 200 calories from soda is not nutritionally equal to 200 calories from nuts.
- Macronutrients: Lists carbs, protein, fats (including saturated/trans), fiber, and sugars.
- % Daily Value (%DV): Based on a 2,000-calorie diet.
- 5% DV or less = low.
- 20% DV or more = high.
- Added sugars: Identified separately—aim for low amounts.
- Vitamins & minerals: Includes vitamin D, calcium, iron, and potassium to highlight common nutrient deficiencies .
Ingredient List
- Ordered by weight, from most to least.
- Choose products where whole foods (e.g., oats) appear near the top.
- Watch for added sugars under different names (syrup, dextrose, cane juice).
- Shorter ingredient lists often indicate less processed foods .
Allergen Warnings
- Required for top allergens: milk, peanuts, wheat, soy, and sesame (added in 2023).
- Appear as “Contains: [allergen]” or in parentheses within the ingredient list.
- Statements like “may contain” or “processed in a facility with…” signal possible cross-contamination .
Front-of-Package (FOP) Labels
Quick visual aids such as:
- Traffic light systems (green = healthier, red = high in sugar/fat/salt).
- Nutri-Score (A–E) and Health Star Rating (0.5–5 stars).
- Warning labels in some countries highlight high sugar, salt, or fat.
- Facts Up Front (U.S.) provides calories and key nutrients on the front.
Tip: FOP labels are helpful, but always confirm with the full Nutrition Facts panel .
Nutrient Content Claims
- Low fat: ≤ 3 g fat per serving.
- Sugar-free: < 0.5 g sugar per serving.
- Good source: 10–19% DV.
- High in: ≥ 20% DV.
⚠️ Terms like “light” may only refer to flavor or color, not nutrient quality .
Health & Structure/Function Claims
- Health claims: Link nutrients to reduced disease risk (e.g., “Low sodium may reduce high blood pressure”). Must be approved.
- Structure/function claims: Describe normal roles of nutrients (e.g., “Calcium supports bone health”). Do not need pre-approval but must be truthful.
- These are often used in marketing—helpful, but should not replace full label evaluation .
Common Misconceptions and Challenges
- Serving Size Confusion
- Many consumers underestimate servings.
- Example: A pint of ice cream labeled “200 calories/serving” with 3 servings = 600 calories if eaten whole.
- Some updated labels now list per container totals to reduce this error .
- “Health Halo” Claims
- Words like natural, organic, low-fat, sugar-free, no added sugar can mislead.
- “Low-fat” foods often have extra sugar.
- “Sugar-free” products may still have calories and carbs.
- “No added sugar” foods may still be high in natural sugars (fruit juice).
Tip: Ignore buzzwords; read the ingredient list and Nutrition Facts .
- Nutrient Profile Bias
- Focusing only on one claim like “gluten-free” or “organic” ignores the whole profile.
- Gluten-free cookies can still be high in sugar and fat.
- “0 trans fat” or “cholesterol-free” does not mean heart-healthy if the food is high in sodium or saturated fat.
Tip: Always assess both nutrients to limit (sodium, sugar, saturated fat) and nutrients to increase (fiber, vitamins, minerals) .
Label Literacy and Consumer Understanding
Studies show that:
- Confusion is common: Many misinterpret serving sizes and %DV.
- Education improves choices: Teens who learned label use ate more fruit and fewer sugary drinks.
- Trust matters: Consumers may blindly accept claims from trusted brands or ignore valid info if skeptical.
- Buzzwords mislead: Terms like “clean” or “natural” create a false sense of healthiness .
Coaching Strategies for Label Reading
- Education: Teach clients to focus on critical areas (calories, serving size, protein, fiber).
- Personalization: Tailor label use to conditions like hypertension (low sodium) or diabetes (carb awareness).
- Shopping practice: Encourage clients to compare labels across products before choosing.
- Emphasis: Even seemingly healthy foods require label reading—health halos can mask unhealthy nutrient profiles .
Conclusion
Food labels are powerful tools for informed eating. By learning to interpret serving sizes, %DV, and ingredients—while avoiding traps like health halos—consumers can make healthier, evidence-based decisions. With growing use of added sugar labeling, clearer serving sizes, and digital tools, label literacy will only improve. Coaches play a vital role in teaching clients to look beyond marketing and trust the facts .
Study Guide – Chapter 13: Dietary Guidelines
Introduction
Dietary guidelines provide science-based nutrition advice to help people improve health and prevent chronic diseases like obesity, diabetes, and heart disease. They shape public policy, education, and individual food choices. Over time, the focus has shifted from preventing nutrient deficiencies to promoting long-term health and disease prevention .
Evolution of Guidelines
- 1894: USDA’s first nutrition advice stressed variety, balance, and moderation.
- 1916–1920s: Early food group guides emphasized milk/meat, cereals, fruits/vegetables, fats, and sugars.
- 1941: First RDAs (Recommended Dietary Allowances) established for vitamins and protein.
- WWII (1940s): “Basic 7” food groups supported rationing.
- 1956–1992: “Basic Four” food groups (milk, meat, fruits/vegetables, grains).
- 1980: First Dietary Guidelines for Americans (DGA), focusing on moderation and chronic disease prevention.
- 1992: USDA Food Pyramid emphasized grains at the base.
- 2011: MyPlate replaced the pyramid with a simple plate visual.
- 2020–2025: Current guidelines stress nutrient-dense foods, limiting added sugars, and customizing diets .
Key shift: From treating deficiencies → to addressing chronic disease risk and overall eating patterns .
2020–2025 U.S. Guidelines: Core Principles
- Healthy Eating Pattern Across Life Stages
- Infants: Breastfeed exclusively for ~6 months; introduce nutrient-rich foods at 6 months.
- All ages: Emphasize vegetables, fruits, whole grains, lean protein, and healthy fats .
- Customization
- Adapt to cultural, personal, and budget needs.
- Supports flexibility (Mediterranean, vegetarian, or traditional diets) .
- Food Group Goals (Nutrient-Dense Choices)
- Vegetables: ~2½ cups/day.
- Fruits: ~2 cups/day.
- Grains: ~6 oz/day (half whole grains).
- Protein: ~5½ oz/day.
- Dairy: ~3 cups/day (or soy alternatives).
- Oils: ~27 g/day.
- Prioritize whole fruits, whole grains, lean proteins, and low-fat dairy .
- Limits on Nutrients of Concern
- Added sugars: <10% of calories (0% for <2 yrs).
- Saturated fat: <10% of calories.
- Sodium: <2,300 mg/day.
- Alcohol: Not recommended; if consumed, ≤1 drink/day (women), ≤2 (men). None in pregnancy .
Tools for Application
The Food Pyramid (1992–2010)
- Grains at base (6–11 servings/day), fruits/vegetables in middle, proteins/dairy above, fats/sweets at tip.
- Messages: variety, grains as the foundation, moderate protein/dairy, limit fats/sweets.
- Criticisms: Didn’t distinguish whole vs. refined grains, healthy vs. unhealthy fats. Overemphasis on “low fat” led to higher refined carb intake .
MyPlate (2011–Present)
- Visual: Half the plate fruits/vegetables, ¼ grains, ¼ protein, side circle for dairy.
- Benefits: Simple, visual, adaptable across cultures, emphasizes balance.
- Limitations: Doesn’t show oils/sugars, and lacks detail on quality within groups. Requires added education to promote nutrient-dense choices .
Nutrient Density
Central to the 2020–2025 guidelines: “make every bite count.”
- Nutrient-dense foods = high vitamins, minerals, fiber, and lean protein with minimal added sugar, sodium, or unhealthy fat.
- Examples: Vegetables, fruits, whole grains, lean proteins, nuts, low-fat dairy.
- Prioritize cooking methods like grilling/steaming over frying.
- Avoid empty-calorie items like soda, candy, and fried foods .
Life Stage Guidance
For the first time, guidelines include specific recommendations by age group:
- Infants (0–2 yrs): Exclusive breastfeeding for 6 months; introduce iron-rich foods at 6 months; avoid added sugars/honey; early allergen exposure may lower allergy risk.
- Children & Teens (2–18 yrs): Emphasize nutrient-dense foods, limit sugary snacks/drinks, ensure calcium, vitamin D, iron, and protein; encourage ≥60 min/day activity.
- Adults (19–59 yrs): Plant-forward diets with fiber, lean protein, healthy fats. Portion control and exercise (150 min/week). Women of childbearing age: adequate folate and iron.
- Older Adults (60+): Nutrient needs remain high though calories decline; emphasize protein, fiber, hydration, vitamin D, B12, potassium. Adjust textures/flavors for appetite/digestion.
- Pregnancy/Lactation: Higher needs for folate, iron, calcium, vitamin D, iodine, omega-3s. Avoid high-mercury fish, unpasteurized foods, and alcohol .
Public Perception & Misinformation
Several myths create confusion:
- “Guidelines keep changing, so they can’t be trusted” → Core advice has been stable (fruits, vegetables, whole grains, lean proteins). Updates reflect better science.
- “They’re controlled by industry” → Developed by independent expert panels with public input.
- “They don’t apply if I have a condition” → Guidelines are for everyone, including most with chronic diseases.
- “Low-fat guidelines caused obesity” → Obesity rise tied more to inactivity, processed foods, and misapplication of advice.
- “Nutrition science is unreliable” → Guidelines reflect decades of evidence, not single studies .
Conclusion
Dietary guidelines have evolved from fighting deficiencies to guiding lifelong healthy eating. The 2020–2025 edition highlights nutrient-dense foods, plant-based patterns, cultural flexibility, and life stage–specific recommendations. Tools like MyPlate translate science into action.
Though nutrition science evolves, the core message is consistent: eat a variety of wholesome foods, limit added sugars, sodium, and unhealthy fats, and make each bite count.
Study Guide – Chapter 14: Specialty Diets
Introduction
There is no single “best” diet for everyone. Success depends on core principles: calorie balance, macronutrient composition, micronutrient sufficiency, food quality, and sustainability. Popular specialty diets like the Mediterranean, intermittent fasting, Paleo, vegetarian/vegan, keto, and fad diets all have pros and cons. Coaches should evaluate diets for nutritional adequacy, evidence-based benefits, and long-term adherence .
Mediterranean Diet
- Definition: Traditional eating style from Greece, Italy, Spain. Emphasizes vegetables, fruits, legumes, nuts, seeds, whole grains, olive oil, fish, with limited dairy, poultry, and red meat. Optional moderate wine. Also encourages cooking at home and shared meals .
- Benefits: Lowers risk of heart disease, stroke, hypertension, diabetes, and Alzheimer’s. Promotes longevity and reduced inflammation. Eco-friendly and flexible .
- Challenges: Cost/access to fresh foods and olive oil may be barriers. Adaptations include frozen produce or other plant oils. Athletes may need extra protein/calories .
Intermittent Fasting (IF)
- Definition: Focuses on when you eat, not what. Methods include:
- Time-restricted feeding (TRF): 16:8, 14:10 eating windows.
- 5:2 diet: Two low-calorie days per week.
- Alternate-day fasting.
- Benefits: Can support weight loss, blood sugar control, improved insulin sensitivity, cholesterol, and possibly inflammation. Many find it simplifies eating .
- Challenges: Hunger, fatigue, irritability, and social disruption. Not suitable for children, teens, pregnant women, or people with eating disorders. Needs balanced meals to avoid nutrient gaps. Athletes may struggle with energy for high-intensity training .
Paleolithic (Paleo) Diet
- Definition: Based on presumed ancestral diets. Includes lean meats, fish, eggs, fruits, vegetables, nuts, seeds. Excludes grains, legumes, dairy, refined sugar, and processed foods .
- Benefits: May reduce weight, blood sugar, cholesterol, and blood pressure. High protein promotes satiety and muscle retention .
- Challenges: Eliminates nutrient-rich foods like dairy, legumes, and whole grains → risk of calcium, vitamin D, fiber, and B vitamin deficiencies. Can be costly, socially limiting, and misapplied as a high-meat diet. A modified version (allowing legumes or dairy) is often more sustainable .
Vegetarian & Vegan Diets
- Definition:
- Vegetarian variations: lacto-ovo, lacto, ovo, pescatarian, flexitarian.
- Vegan: excludes all animal products (including honey).
- Benefits: Linked to lower risk of heart disease, diabetes, hypertension, some cancers, and lower BMI. High fiber, antioxidants, and phytochemicals. Environmentally sustainable .
- Challenges/Nutrient Risks:
- Vitamin B12: Absent from plants → must use fortified foods or supplements.
- Iron: Non-heme iron absorbed less efficiently; pair with vitamin C sources.
- Zinc & Calcium: May require fortified foods.
- Vitamin D & Omega-3s (EPA/DHA): Often need supplementation.
- Protein: Quality varies—variety needed (legumes, grains, soy, nuts).
- Iodine & Selenium: Monitor intake; use iodized salt, Brazil nuts .
- Athletes: Endurance often supported by higher carbs; strength athletes must ensure adequate protein and may supplement creatine .
Ketogenic (Keto) Diet
- Definition: Very low-carb, high-fat diet (70–75% fat, 20–25% protein, 5–10% carbs; <50 g/day). Promotes ketosis, where fat/ketones fuel the body .
- Benefits: Effective for drug-resistant epilepsy; can aid short-term fat loss, lower triglycerides, raise HDL, improve insulin sensitivity, and reduce HbA1c in type 2 diabetes. Early evidence suggests possible benefits for PCOS, fatty liver disease, and neurological disorders .
- Challenges: Low adherence long term. Side effects include “keto flu” (fatigue, headaches). Risks of nutrient deficiencies (fiber, magnesium, folate, vitamin C, vitamin K, calcium, vitamin D). Some may see LDL cholesterol increases. Social and lifestyle barriers are significant. Must use unsaturated fats and non-starchy veggies for safety .
Fad Diets
- Definition: Trendy, restrictive diets with big promises and little science (e.g., detox cleanses, carnivore diet, grapefruit diet). Often cut out entire food groups or push expensive products .
- Risks: Short-term weight loss usually from calorie restriction, not special effects. Lead to nutrient deficiencies, muscle loss, dehydration, and weight cycling (yo-yo dieting). Harmful to relationship with food; promote guilt, bingeing, and unrealistic expectations .
- Public Perception: Thrive on pseudoscience, emotional marketing, and social media buzzwords (“detox,” “fat-burning mode”). Accessibility is also an issue—many require costly specialty products .
- Coaching Role: Teach clients to spot red flags: promises of quick results, elimination of food groups, lack of scientific evidence .
Key Takeaways
- No single “best” diet—effectiveness depends on adherence, nutrient adequacy, and individual preference.
- Successful diets (Mediterranean, plant-based, moderate low-carb) share common themes: whole foods, vegetables, adequate protein, minimal processed foods.
- Coaches should focus on principles over labels, tailoring diets to client goals, culture, health status, and lifestyle.
- Sustainable results come from realistic, balanced habits—not extreme restrictions or fads.
Study Guide – Chapter 15: Goal Setting
Introduction
Goal setting is a cornerstone of nutrition coaching. It transforms vague intentions (“I want to be healthier”) into specific, actionable steps. Effective goals provide direction, motivation, accountability, and structure, making it easier for clients to adopt and sustain new behaviors .
Theoretical Foundations
Psychologists Locke and Latham’s Goal-Setting Theory shows that specific and challenging goals outperform vague or easy ones. For example, “eat 5 servings of vegetables daily” is more effective than “eat healthier.” Goals boost motivation, effort, and persistence when they are realistic and achievable .
Functions of Goal Setting
- Clarifies direction: Defines success (e.g., “exercise 4x per week for 30 minutes”).
- Increases motivation: Benchmarks encourage continued effort.
- Creates accountability: Measurable, time-bound goals let coaches and clients track progress objectively .
Types of Goals
- Outcome Goals – Focus on results (e.g., “lose 30 pounds in 6 months”). Motivating, but influenced by outside factors (genetics, water weight). Best used for long-term direction.
- Performance Goals – Specific, controllable actions (e.g., “exercise 5x per week,” “track calories daily”). Directly influence outcomes, maintain confidence, and support long-term success.
- Process Goals – Small, daily habits (e.g., “pack lunch daily,” “replace soda with water”). Fully controllable and build consistency.
Best practice: Emphasize process and performance goals as the foundation, while treating outcome goals as secondary .
SMART Goals
The SMART framework refines goals to make them practical:
- Specific – Clearly defined (e.g., “3 servings of vegetables daily”).
- Measurable – Trackable (e.g., “8 cups of water/day”).
- Achievable – Realistic given client’s resources.
- Relevant – Connected to personal values (e.g., weight loss for health, not just appearance).
- Time-bound – With deadlines or timeframes.
Example: Instead of “eat better,” a SMART goal is: “Bring a homemade lunch with lean protein and vegetables to work 3 of 5 days each week for 8 weeks.” SMART goals consistently outperform vague intentions .
Goal-Setting Process
- Clarify motivation – Understand why the goal matters.
- Create a SMART goal – Refine until all five elements are included.
- Write it down – Increases accountability and recall.
- Develop an action plan – Break into steps (meal planning, shopping, prepping).
- Set milestones – Break large goals into short-term checkpoints.
- Act and track – Use logs, apps, or calendars.
- Reevaluate and adjust – Celebrate wins, learn from setbacks, modify if needed .
Reevaluation and Feedback
- Celebrate successes: Reinforces confidence and motivation.
- Address challenges: Explore barriers like time, stress, or resources.
- Adjust expectations/strategies: Make goals easier or harder as appropriate.
- Reframe failure as feedback: Missed goals reveal obstacles, not personal flaws.
- Renew motivation: Reconnect with the client’s “why” (e.g., more energy, better sleep) .
Why Goals Work (Mechanisms)
Goals influence behavior through four psychological processes:
- Focused attention – Directs awareness to goal-related choices.
- Effort mobilization – Encourages greater effort (specific benchmarks push harder).
- Persistence – Promotes consistency despite challenges.
- Learning & strategy adaptation – Encourages problem-solving when barriers arise .
Behavioral Strategies for Success
- Self-monitoring: Tracking food, activity, or weight increases awareness and adherence. Apps, journals, and fitness trackers help.
- Incremental changes: Break large goals into small steps (e.g., reduce 100 calories/day instead of 500). Small wins build momentum.
- Social support & accountability: Involving friends, family, or groups boosts success. “Accountability buddies” and weekly check-ins reinforce consistency .
Overcoming Barriers
Common obstacles include:
- Overly ambitious goals – Break down into smaller steps.
- Lack of autonomy – Let clients co-create goals for ownership.
- Inconsistent follow-up – Regular check-ins prevent drift.
- Psychological resistance – Address fear of failure, self-sabotage, or negative thoughts.
- Practical barriers – Time, money, or access to resources. Coaches can provide solutions like quick meals or budget strategies.
- Supportive environment & CBT tools – Use positive self-talk, “if-then” plans, and stress-coping strategies .
Emotional and Motivational Factors
- Unmet goals can trigger guilt and low confidence. Coaches should normalize setbacks and encourage a growth mindset.
- Self-compassion helps clients bounce back faster after slips.
- Resilience develops through celebrating small wins and maintaining progress identity.
- After success: Set new goals to sustain motivation; celebrate achievements to reinforce positive behavior .
Best Practices for Coaches
- Personalize goals to fit health needs and culture.
- Use technology for consistent tracking.
- Build supportive environments (family, peer groups).
- Review goals regularly.
- Address mental barriers with motivational interviewing and CBT tools.
This holistic coaching approach increases adherence and long-term success .
Conclusion
Effective goal setting connects knowledge to action. By using SMART goals, incremental strategies, self-monitoring, and social support, coaches help clients turn intentions into lasting behavior change. The ultimate value of goal setting isn’t just reaching one target but developing lifelong skills to adapt, stay motivated, and maintain health.
Study Guide – Chapter 16: Motivational Interviewing and Stages of Change Theory
Introduction
Behavior change is not linear—it requires both readiness and supportive coaching. Two major tools guide this process:
- Motivational Interviewing (MI): A collaborative, client-centered style that elicits personal motivation.
- Stages of Change (Transtheoretical Model, TTM): A framework describing how people progress through change.
Together, they help coaches move clients from ambivalence to action while respecting autonomy .
Motivational Interviewing (MI)
Definition
MI is a conversational method designed to strengthen a client’s intrinsic motivation for change. Instead of telling clients what to do, the coach draws out their own reasons for change .
Types of Motivation
- Intrinsic: Driven by personal values (e.g., eating veggies for energy). More sustainable.
- Extrinsic: Driven by rewards or external pressure (e.g., dieting for praise). Can spark change but less lasting.
- Self-Determination Theory spectrum: Ranges from amotivation → external regulation → introjected → identified → integrated regulation (most autonomous) .
Spirit of MI
- Collaboration: Coach and client are partners.
- Acceptance & Autonomy: Client’s choices are respected.
- Compassion: Genuine care and trust-building.
- Evocation: Draw out the client’s own reasons to change .
Principles of MI (see diagram on page 4)
- Express empathy – validate experiences.
- Roll with resistance – avoid arguing; explore perspective.
- Develop discrepancy – highlight gap between goals and behaviors.
- Support self-efficacy – reinforce belief in ability to change .
Core Skills (OARS)
- Open-ended questions – encourage reflection.
- Affirmations – highlight strengths.
- Reflections – rephrase to show understanding.
- Summaries – organize and reinforce motivations .
Stages of Change (TTM)
Overview
The TTM views change as a process, not a single event. Clients move through distinct stages:
- Precontemplation (Not Ready): No recognition of problem.
- Coach: Share info gently, build trust.
- Contemplation (Thinking About It): Aware but ambivalent.
- Coach: Explore pros/cons, reflect, avoid rushing.
- Preparation (Getting Ready): Intending to change soon.
- Coach: Create SMART goals, build confidence.
- Action (Doing It): Actively changing behavior.
- Coach: Support, problem-solve, celebrate wins.
- Maintenance (Sustaining): >6 months of consistent behavior.
- Coach: Prevent relapse, reinforce success.
- Relapse: Return to old habits.
- Coach: Stay supportive, normalize setbacks, rebuild motivation.
The chart on page 8 clearly summarizes each stage with mindset, strategy, and example dialogue.
Key Constructs
Decisional Balance
Clients weigh pros and cons of change. Early stages = more cons; later stages = more pros. Coaches can reframe negatives and emphasize benefits .
Self-Efficacy
Belief in ability to change. Builds with small wins, affirmations, and reminders of past success. Higher self-efficacy = lower relapse risk .
Integrating MI + TTM
MI and TTM complement each other:
- TTM = the map (when to act).
- MI = the method (how to act).
Stage-Based MI Strategies
- Precontemplation: Raise awareness, ask permission before sharing info.
- Contemplation: Explore ambivalence, encourage “change talk.”
- Preparation/Action: Build confidence, make plans, problem-solve.
- Maintenance: Focus on relapse prevention, ongoing support .
Coaching Best Practices
- Match techniques to stage of change.
- Foster autonomy and ownership.
- Track progress and celebrate milestones.
- Handle resistance with curiosity, not confrontation .
Conclusion
Motivational Interviewing and the Stages of Change model provide a flexible, evidence-based roadmap for supporting client transformation. By listening, respecting autonomy, and tailoring strategies to each stage, coaches can move clients from ambivalence to sustained change.
Key tips for coaches:
- Assess stage of change.
- Listen for motivation and “change talk.”
- Use OARS and empathetic communication.
- Stay supportive and non-judgmental.
- Adjust strategies to match readiness.
Study Guide – Chapter 17: Overcoming Barriers and Effective Communication
Introduction
Success in nutrition coaching depends on more than knowledge—it requires effective communication and problem-solving. Coaches must listen deeply, ask strong questions, provide feedback, and help clients overcome barriers such as time, money, emotions, or misinformation. Cultural competence and digital tools also expand coaching reach .
Core Communication Skills
Active Listening
- Pay full attention: eye contact, nodding, no distractions.
- Reflective listening confirms understanding (e.g., “Meal prepping feels overwhelming”).
- Empathy builds trust: “I see how hard it is to balance work and eating well” .
Questioning Techniques
- Use open-ended questions (“What’s your biggest challenge with healthy eating?”).
- Follow-ups explore motivation and barriers.
- Scaling questions (“On a scale of 1–10, how confident are you?”) assess readiness .
Feedback
- Positive feedback motivates (“Great job adding more vegetables this week!”).
- Constructive feedback should be solution-oriented, not critical (“Would smaller goals help next week?”).
- Give feedback promptly for best impact .
Common Client Barriers
Time Constraints
Busy schedules often limit meal prep and exercise.
Solutions: Teach batch cooking, quick recipes, or meal delivery services .
Financial Limitations
Healthy food or gym memberships can seem too expensive.
Solutions: Highlight affordable foods like beans, eggs, frozen vegetables, bulk buys, and coupons .
Emotional or Stress Barriers
Stress, depression, or low confidence may trigger emotional eating.
Solutions: Stress management (breathing, mindfulness, activity), emotional support, and safe, non-judgmental spaces .
Knowledge Gaps & Misinformation
Clients may believe myths (e.g., “fruit is bad because of sugar”).
Solutions: Provide simple evidence-based education, visuals, and critical thinking skills .
Strategies to Overcome Resistance
- Normalize resistance: Assure clients it’s natural to feel unsure.
- Collaborative problem-solving: Let clients design their own solutions.
- Small wins: Break goals into manageable steps (e.g., one extra glass of water/day).
- If–Then planning: “If I’m too tired to cook, then I’ll reheat a freezer meal” .
Addressing Recurring Challenges
- Nutrition misinformation: Respectfully debunk myths, explain why they sound believable, and give reliable resources.
- Low motivation: Use motivational interviewing, connect goals to personal values, and celebrate small wins.
- Setbacks & non-adherence: Normalize lapses, explore causes, and highlight partial wins. Use empathetic language—avoid blame (see graphic on page 8, which contrasts supportive vs. harmful responses).
- Time limitations: Streamline sessions, use apps or food logs between meetings, and teach quick meal strategies .
Coaching Across Populations
Athletes
- Align meals with training schedules.
- Teach carb fueling, protein recovery, hydration.
- Correct myths (e.g., too much protein).
- Use SMART goals (eat pre-workout, add anti-inflammatory foods).
- Impact: Better performance, recovery, and long-term health .
Older Adults
- Address reduced appetite, mobility issues, or loneliness.
- Ensure adequate calories, protein, vitamin D, and B12.
- Suggest soft/affordable foods, set meal routines, involve caregivers.
- Impact: Better nutrition, mood, independence .
College Students
- Help navigate dining halls, dorm cooking, tight budgets.
- Offer quick, simple recipes and tech-based reminders.
- Link nutrition to immediate benefits (energy, focus).
- Encourage group coaching or peer support.
- Impact: Builds lifelong healthy habits .
Children & Picky Eaters
- Work through parents: encourage pressure-free exposure, family meals, and fun routines.
- Small goals (taste one new veggie/week).
- Celebrate wins with non-food rewards like stickers.
- Involve kids in choosing or preparing foods.
- Impact: Reduces mealtime stress and fosters healthy lifelong eating .
Conclusion
Effective coaching blends science, empathy, and adaptability. Success comes from:
- Listening actively, asking powerful questions, and providing constructive feedback.
- Overcoming barriers with time management, budget solutions, stress support, and education.
- Adjusting strategies for specific populations—athletes, older adults, students, and children.
Even with technology (apps, video calls), human connection remains central. Coaches who adapt to barriers and use strong communication empower clients to build lasting, realistic habits.
Study Guide – Chapter 18: Influence of Stress, Sleep, and Environment on Food Choices
Introduction
Food choices are shaped not only by calories, macronutrients, or diet quality but also by stress, sleep, and environmental context. These external factors alter appetite, cravings, and decision-making, often driving unhealthy patterns. Coaches must understand how these influences interact to guide clients toward sustainable eating habits .
Stress and Food Choices
Why Stress Triggers Eating
- HPA axis activation: Raises cortisol, increasing hunger and cravings—especially for sugary, fatty “comfort foods.”
- Short-term relief: Eating reduces stress temporarily but reinforces emotional eating habits.
- Brain changes: Stress activates reward/emotion centers (dopamine pathways) while weakening self-control, making junk food harder to resist .
Mechanisms
- Cortisol and Cravings: Chronic stress → higher cortisol → preference for high-fat, high-sugar foods.
- Emotional Eating: Using food to cope can become automatic over time.
- Environmental Triggers: Work deadlines, money worries, or social struggles often pair with easy access to fast food or vending snacks .
Health Impacts
Stress eating raises risk of abdominal obesity, metabolic syndrome, diabetes, and heart disease. Long-term patterns worsen insulin resistance, cholesterol, and blood pressure .
Sleep and Food Choices
How Sleep Deprivation Alters Eating
- Hormone imbalance: Less sleep ↓ leptin (satiety), ↑ ghrelin (hunger). Endocannabinoids also rise, increasing food pleasure.
- Brain changes: The prefrontal cortex (self-control) becomes less active, while the amygdala/striatum (reward/emotions) become overactive—similar to stress or intoxication .
- Extended eating window: More hours awake = more opportunities to snack, usually late at night.
Effects on Diet
- Higher cravings for sugar and processed foods.
- Increased daily intake (200–500 kcal more).
- Greater risk of obesity, insulin resistance, and poor diet quality (fewer vegetables, more ultra-processed foods).
Long-Term Consequences
Short sleep (<6 hrs) is linked to weight gain, hypertension, diabetes, and cardiovascular disease. Consistent 7–9 hrs supports appetite control, fewer cravings, and better food choices .
Environmental Influences
- Food Access (Food Deserts): Areas with limited fresh produce force reliance on cheap, processed foods. Raises obesity and chronic disease risk .
- Cost of Food: Healthy foods often cost more. Financial stress drives families toward filling but nutrient-poor fast foods.
- Culture and Traditions: Traditions shape diets positively (e.g., Mediterranean) or negatively (e.g., salt- or fat-heavy dishes). Immigrants often shift toward Western processed foods.
- Marketing & Media: Food ads—especially in low-income/minority areas—promote soda, fast food, and snacks. Kids and adults normalize unhealthy eating when constantly exposed .
Strategies for Coaches
1. Manage Stress Without Food
- Teach relaxation: meditation, breathing, yoga, journaling.
- Encourage exercise as a natural stress reliever.
- Replace stress eating with alternatives (calling a friend, walking).
- For severe emotional eating, suggest counseling .
2. Improve Sleep Hygiene
- Aim for 7–9 hrs/night.
- Keep consistent bed/wake times.
- Limit caffeine, alcohol, and screen use before bed.
- Create a relaxing pre-bed routine and cool, dark sleep environment .
3. Create a Supportive Food Environment
- Stock healthy snacks at home and keep junk out of sight.
- Prep meals in advance to reduce fast-food reliance.
- Use local resources (farmer’s markets, produce delivery).
- Advocate for healthier work/school/community options.
- Help clients mute or avoid junk food ads .
4. Educate and Empower Clients
- Explain how stress and sleep affect hormones like cortisol, leptin, and ghrelin.
- Teach skills: meal prep, budgeting, label reading.
- Plan ahead for challenges (healthy lunches, travel snacks).
- Encourage group support or community classes for cooking and stress relief .
Conclusion
Healthy eating requires more than willpower—it’s shaped by stress, sleep, and environment:
- Stress boosts cravings and emotional eating.
- Poor sleep disrupts hunger hormones and weakens decision-making.
- Environment (food access, culture, marketing) influences default choices.
Coaches should take a holistic approach, combining stress management, sleep support, and environmental strategies with nutrition education. This balance helps clients form sustainable habits, overcome barriers, and make healthy eating feel natural.
Study Guide – Chapter 19: Tracking Client Progress and Adjusting Plans
Introduction
Nutrition coaching doesn’t stop at making a meal plan—success requires tracking, assessment, and ongoing adjustments. Progress monitoring provides motivation, accountability, and objective data, while tailored modifications ensure plans remain effective and sustainable .
Importance of Tracking
- Encourages accountability and self-awareness.
- Allows for evidence-based decisions.
- Enhances adherence and results, especially when combined with professional guidance.
- Research shows clients using apps + coaching achieve better outcomes in weight, waist circumference, and metabolic health than self-monitoring alone .
Methods of Tracking Progress
1. Dietary Logs
- Written journals or apps (e.g., MyFitnessPal).
- Useful for identifying nutrient gaps (e.g., low protein, high sugar).
- Requires honesty and consistency .
2. Anthropometric Measurements
- Weight, body fat %, waist/hip/chest circumference.
- Waist circumference is particularly valuable for metabolic risk.
- Should be taken consistently (same time of day, same conditions).
- Combining different methods gives a clearer picture .
- See page 4 infographic: methods include skinfold calipers, bioelectrical impedance, DEXA, MRI, underwater weighing, waist-to-hip ratio, and more.
3. Biomarkers
- Lab tests: blood glucose, cholesterol, triglycerides, blood pressure, vitamin status.
- Objective proof of health improvements when physical changes are slow.
- Example: HbA1c drop shows improved glycemic control .
4. Behavior & Lifestyle Assessments
- Sleep, hydration, stress, physical activity.
- Journals and weekly check-ins reveal patterns (e.g., poor sleep → overeating).
5. Technology & Wearables
- Track steps, HR, sleep, activity.
- Boost accountability and give real-time insights when synced with food logs.
- Must be used mindfully to avoid obsession .
Data Interpretation & Adjustment Strategies
1. Set SMART Data-Based Goals
Use data to make goals specific and measurable (e.g., “Add 30g more protein/day” instead of “eat better”) .
2. Adjust Caloric Intake
- Weight loss stalls: tighten deficit, check adherence, try calorie cycling, refeeds, or short diet breaks.
- Muscle gain stalls: increase 250–300 kcal/day.
- Always adjust gradually .
3. Modify Macronutrient Ratios
- Increase protein (1.2–2.0 g/kg) for satiety, recovery, and lean mass.
- Adjust carbs around workouts for energy.
- Adjust fats for hormones and satiety .
4. Refine Meal Timing & Frequency
- Front-loading calories earlier in the day may help weight loss and blood sugar.
- Encourage consistent eating patterns (avoid late-night snacking).
- Time-restricted feeding (8–10 hr window) can aid adherence .
5. Enhance Accountability with Technology
- Habit trackers, food apps, reminders.
- Progress photos, fitness assessments.
- Helps sustain adherence .
Best Practices for Adjusting Nutrition Plans
- Regular Reviews: Weekly/biweekly check-ins.
- Data-Driven Adjustments: Only change when progress stalls or issues arise.
- Non-Scale Victories: Celebrate energy, sleep, performance, and adherence.
- Address Barriers: Solve for time, stress, or environment.
- Personalization: Keep adapting to evolving goals, preferences, and lifestyle .
Troubleshooting Common Challenges
- Plateaus: Normal part of weight loss. Review adherence, portion creep, and adjust intake or activity. Add strength training.
- Inconsistent Tracking: Simplify—use photo logs or partial tracking (2–3 days/week). Normalize lapses.
- Motivation Dips: Reconnect with “why,” set small wins, try challenges, and use motivational interviewing .
The chart on page 10 highlights:
- Plateau → unchanged weight → adjust calories/activity.
- Motivation dip → low enthusiasm → reset goals, reinforce positives.
- Inconsistent logging → missing entries → simplify, set reminders .
Case Studies
1. Breaking a Weight Loss Plateau
- Client: 35-year-old male aiming to lose 15 lb in 3 months.
- Issue: Only 2 lb lost in 4 weeks due to weekend takeout, logging gaps, and hunger.
- Adjustments:
- Calorie cycling (refeed day on weekends).
- Higher protein + fiber for satiety.
- Simpler meal prep + healthy takeout options.
- Flexible workouts (short home circuits).
- Photo logging + motivational texts.
- Outcome: Broke plateau, lost 7 lb by 8 weeks .
2. Optimizing Muscle Gain
- Client: 28-year-old female, goal = +5–6 lb lean mass.
- Issue: Surplus too low, high satiety limited intake.
- Adjustments:
- Added calorie-dense foods (nuts, oils, shakes).
- Reduced protein slightly, raised fats for easier calories.
- Consistent meal/snack timing.
- Added creatine and strength tracking.
- Outcome: +5.5 lb weight in 16 weeks, with strong performance gains .
3. Improving Metabolic Health
- Client: 50-year-old male with prediabetes.
- Issue: Low energy from long fasting, evening cravings, food log fatigue.
- Adjustments:
- Slightly widened eating window to include small evening snack.
- Encouraged Omega-3s, plant sterols, fiber.
- Added light jogging intervals.
- Reduced logging frequency to 1–2 days/week.
- Outcome: HbA1c dropped from 6.1% to 5.4%, LDL to 95 mg/dL, BP to 120/78. Weight -12 lb .
Conclusion
Tracking is the engine of progress in coaching. Using multiple tools (logs, biometrics, body comp, wearables) gives a complete picture, while interpreting and adjusting data ensures plans evolve. By combining science with empathy, coaches keep clients engaged, adaptable, and moving toward lasting success.
Study Guide – Chapter 20: Dietary Assessment
Introduction
Dietary assessment is the foundation of both research and clinical nutrition practice. It evaluates what and how much people eat, helping identify nutrient gaps, track progress, and guide interventions. Within the Nutrition Care Process (NCP), it falls under the first step—assessment—and must be combined with anthropometrics, biochemical data, clinical signs, and client history for a full picture .
Domains of Nutrition Assessment
According to the Academy of Nutrition and Dietetics, five key domains form a comprehensive assessment :
- Food/Nutrition-Related History: Dietary recalls, FFQs, food diaries, supplements, habits, and lifestyle.
- Anthropometric Measurements: Height, weight, BMI, circumferences, body fat, growth charts.
- Biochemical Data: Lab tests like blood sugar, cholesterol, iron, vitamins, hydration, and stool tests (gut health).
- Physical Findings: Observable issues like muscle wasting, swelling, pale skin, brittle nails.
- Client History: Medical, social, cultural, and economic context affecting food access and choices.
Purposes of Dietary Assessment
Dietary assessment serves multiple functions :
- Evaluating Nutritional Status: Spot deficiencies or excesses by comparing intake with guidelines.
- Informing Diagnoses: Identify problems like low protein in wound healing or high sugar in diabetes.
- Tracking Progress: Monitor adherence to plans (e.g., reduced saturated fat, increased fiber).
- Guiding Clinical Decisions: Adjust for intolerances, medications, or supplements.
- Public Health/Policy: Large surveys help shape guidelines and evaluate interventions like sugar taxes.
Major Assessment Methods
1. 24-Hour Recalls
- Strengths: Detailed, low burden, short memory window, flexible for research/clinical use.
- Limitations: Recall bias, atypical days, resource-intensive.
- Best practice: Use multiple recalls (weekday + weekend), trained interviewers, visual aids, and validation methods like doubly labeled water .
2. Food Frequency Questionnaires (FFQs)
- Strengths: Low cost, good for long-term habits and large studies, self-administered.
- Limitations: Fixed food lists, poor portion accuracy, underestimates energy/nutrients.
- Best use: Ranking intake across populations, not precise measurement.
3. Food Records/Diaries
- Strengths: Real-time, detailed, accurate, raises self-awareness.
- Limitations: Time-consuming, burdensome, can change behavior (reactivity).
- Best use: Motivated clients, research requiring precision.
- Tip: Apps with barcodes/photos reduce burden.
4. Diet History Interviews
- Strengths: Comprehensive, contextual, good for counseling.
- Limitations: Time-intensive, qualitative, interviewer variability.
- Best use: First clinical visits, combined with other methods.
5. Emerging Digital Tools
- Image-based methods: Meal photos before/after eating. Reduce memory error, but depend on photo quality.
- Wearables: Sensors track bites, chewing, or glucose. Still emerging.
- Apps: Easy logging with databases/barcodes. Data quality varies.
- Integration: Combining tools (apps + recalls + wearables) gives the best accuracy .
Critical Issues in Dietary Assessment
Misreporting
- Underreporting (common in higher BMI clients) hides overeating; often driven by social desirability.
- Misreporting: Forgotten or misjudged portions; “phantom” vs. “missing” foods.
- Solutions:
- Create a nonjudgmental space.
- Use multiple passes in recalls.
- Provide visual aids/apps for portion sizes.
- Validate with objective data (labs, doubly labeled water).
- Focus on patterns, not perfection—habits matter more than exact calories .
Best Practices for Coaches
- Combine Methods: Multiple tools (recall + labs + anthropometrics).
- Educate Clients: Stress honesty and accuracy.
- Cultural Sensitivity: Adapt to traditions and preferences.
- Regular Monitoring: Repeat assessments to track progress and adjust plans .
Pulling It All Together
No single tool gives the whole story. For example:
- A recall shows low protein intake.
- Anthropometrics reveal weight loss.
- Labs confirm low albumin.
- Physical signs show muscle loss.
- Client history reveals limited cooking skills.
Together, these domains provide a complete picture, guiding targeted interventions like protein supplementation or meal prep strategies .
Conclusion
Dietary assessment blends science and communication skills. It requires choosing the right methods, minimizing misreporting, and integrating multiple data sources. When done well, it drives effective nutrition interventions and supports both individual health outcomes and public policy.
Key takeaway: No single method is enough—accuracy comes from combining tools, context, and empathy.
Study Guide – Chapter 21: Navigating Diet Pitfalls
Introduction
Only about 20% of overweight individuals maintain long-term weight loss, showing how common it is to fall into “diet pitfalls.” These challenges come from psychological, environmental, social, and behavioral factors that derail progress. Recognizing pitfalls and applying evidence-based strategies helps people build lasting, flexible nutrition habits .
Common Diet Pitfalls
- Psychological Barriers & Emotional Eating
- Stress, anxiety, or depression → cravings for high-calorie comfort foods.
- Eating for emotions, not hunger, causes guilt and weight gain.
- Strategy: Identify triggers, develop healthier coping mechanisms .
- Environmental & Social Influences
- Food deserts, fast food availability, peer pressure, and social events encourage poor eating.
- Strategy: Change surroundings (stock healthy snacks, plan social outings without junk food) .
- Lack of Nutrition Knowledge
- Misleading marketing (“low-fat,” “gluten-free”) or fad myths create confusion.
- Strategy: Teach fundamentals—label reading, portion sizes, food group balance .
- Poor Meal Planning
- Skipping prep leads to fast food reliance or overeating later.
- Strategy: Grocery lists, prepping meals/snacks ahead of time .
- Unrealistic Goals & Motivation Swings
- Yo-yo dieting often comes from unsustainable, overly ambitious targets.
- Strategy: Set realistic, flexible goals, link them to intrinsic motivators (energy, mood) .
Evidence-Based Interventions
- Professional Counseling: Personalized coaching boosts accountability and adherence. Programs like the Diabetes Prevention Program show improved weight and blood sugar control .
- Technology Tools: Mobile apps, trackers, and reminders improve weight loss outcomes. Meta-analyses confirm diet app users lose more weight than non-users .
- Public Health Policies: Nutrition labeling, soda taxes, and restrictions on junk food ads reshape food environments. As shown on page 5 pyramid, lasting habits require education, environment, social support, coping strategies, and personalization .
Red Flags to Avoid
- Overly Restrictive Diets
- Risks: Nutrient deficiencies, binge eating, slowed metabolism, hormonal issues.
- Solution: Moderate calorie deficits (300–500/day), balanced macronutrients, steady progress .
- Fad Diets
- Risks: Yo-yo dieting, lack of sustainability, nutrient gaps.
- Solution: Prioritize long-term behavior change; keep positive aspects (e.g., more veggies) but reject extremes .
- Ignoring Individual Needs
- Risks: Poor adherence, worsening of health issues (e.g., high-protein diets with kidney disease).
- Solution: Personalize to age, culture, medical history, preferences .
- Neglecting Behavior Factors
- Risks: Stress eating, mindless snacking, relapse.
- Solution: Use self-monitoring, CBT, mindfulness, food/mood journaling .
Strategies for Overcoming Pitfalls
- Nutrition Education – Teach food labels, portion sizes, nutrient-dense vs calorie-dense foods.
- Realistic Expectations – Emphasize gradual change, highlight non-scale victories.
- Social Support – Family, friends, or online groups increase accountability and resilience.
- Planning & Preparation – Meal prep, lists, batch cooking, and snack strategies.
- Coping with Emotional Eating – Replace stress eating with mindfulness, journaling, exercise, or therapy .
Additional Barriers
- Behavioral & Environmental: Time, money, access, peer pressure, and cooking skills. Practical solutions include pre-cut produce, affordable recipes, and healthier cafeteria policies .
- Emotional & Psychological: Processed, high-sugar diets worsen depression/anxiety; balanced diets improve mood. The Food-Mood chart on page 13 shows the link between diet and mental health .
- Public Health Messaging: Weight-focused campaigns can backfire, causing stigma. Positive, weight-neutral approaches (body positivity, cooking, movement) improve adherence .
- Personalized Nutrition: Genetics, metabolism, microbiome, and culture shape diet response. Precision nutrition ensures better adherence and outcomes .
Role of Nutrition Coaches
- Accountability: Check-ins help problem-solve and build consistency.
- Flexibility: Teach clients to adapt plans for real life (holidays, stress).
- Empowerment: Equip clients with knowledge and skills for long-term independence.
Nutrition coaches turn setbacks into learning opportunities and help clients develop self-sufficiency in managing habits .
Conclusion
Navigating diet pitfalls requires education, flexibility, support, and personalization. Success isn’t measured just by weight loss but by energy, health, and relationship with food. With coaching, clients learn to avoid restrictive fads, manage stress eating, and tailor nutrition to their lives—transforming obstacles into lasting, enjoyable habits.
Study Guide – Chapter 22: Practical Nutrition Programming for Clients
Introduction
Nutrition programming translates nutrition science into personalized, actionable plans. Effective coaching combines individual assessment, behavioral change strategies, energy balance, structured follow-ups, and tailored applications for general clients and athletes. The goal is to build lasting, adaptable habits .
Key Principles of Nutrition Programming
- Individualization & Client-Centered Approach
- Assess diet history, labs, body metrics, and lifestyle.
- Respect cultural preferences, schedules, and personal goals.
- Use motivational interviewing to draw out client-driven reasons for change .
- Behavioral Change Tools
- SMART goals: Specific, measurable, realistic targets.
- Self-monitoring: Apps/journals improve awareness and outcomes.
- CBT (Cognitive-Behavioral Therapy): Reframe setbacks, plan for risky situations.
- Motivational interviewing: Boosts motivation, adherence, and weight loss .
- Energy Balance & Nutrient Timing
- Energy balance is fundamental: calories in vs. out.
- Macronutrients:
- Protein: higher intake aids fat loss and muscle retention.
- Carbs: key for endurance.
- Fats: needed for hormone health.
- Nutrient timing: Protein spread throughout day + post-workout; carbs before/during endurance exercise; casein at night for recovery .
- Structured Follow-Ups & Adjustments
- Frequent check-ins → improve adherence.
- Address plateaus, emotional eating, or lifestyle shifts.
- Track beyond weight (energy, sleep, habits).
- Adjust calories, macros, and strategies as needed.
- Wins (e.g., home cooking, better labs) should be reinforced .
Practical Applications
Working with General Populations
- Whole, minimally processed foods: fruits, vegetables, lean proteins, grains, nuts, healthy oils.
- Balanced macronutrients: typically 45–55% carbs, 20–30% protein, 25–35% fat.
- Portion control & mindful eating: plate method, hunger cues, avoid emotional eating.
- Common pitfalls:
- Sugary drinks → swap for water/tea.
- Low fiber → aim for 25–30g/day.
- Lifestyle support: sleep, stress management, daily activity.
- Education: teach label reading, grocery shopping, meal prep .
Nutrition for Athletes
- Adequate energy: Prevent RED-S (low energy availability). Most athletes need 2,500–4,000+ kcal/day, adjusted by sport.
- Macronutrients:
- Carbs: 5–10 g/kg/day, plus fuel before/during (30–60g/hr) and recovery (~1–1.2 g/kg).
- Protein: 1.2–2.0 g/kg/day; 20–40g per meal; casein before bed.
- Fat: 15–35% of calories (healthy sources).
- Hydration & electrolytes: Replace 1–1.5 L per kg lost; sodium and electrolytes for long sessions/heat.
- Recovery timing: Protein + carbs within 30–60 min post-exercise; anti-inflammatory foods throughout the day.
- Supplements (when necessary): Iron, vitamin D, omega-3s, creatine, caffeine, beta-alanine—only if diet is sound and safe.
- Periodized nutrition: Match intake to training load; manage phases for weight-class sports .
Case Studies
- Adolescent Obesity
- Profile: 16-year-old, fast food/soda, sedentary.
- Plan: Motivational interviewing, small goals (replace soda, walk/bike to school).
- Results: More fruits/veggies, daily biking, better energy, small BMI drop .
- Elite Athlete with RED-S
- Profile: 22-year-old female runner, under-fueling (~1,800 kcal/day).
- Plan: Increase calories, carbs around workouts, snacks, iron-rich foods, vitamin D & omega-3s.
- Results: Energy restored, regular cycles, fewer injuries, faster recovery, new personal bests .
- Adult Weight Loss
- Profile: Maria, 45, office worker, BMI 31, wants to lose 10–15 lbs.
- Plan: 1,500 kcal/day Mediterranean-style plan (40% carbs, 30% protein, 30% fat), food tracking, walking.
- Results: Lost 12 lbs in 12 weeks, less knee pain, more satiety, overcame plateau with snack swaps & added walking .
Conclusion
Practical nutrition programming is about science + personalization + coaching:
- Assess each client individually.
- Use behavioral strategies (SMART goals, self-monitoring, MI).
- Ensure energy balance, appropriate macros, and (for athletes) nutrient timing.
- Rely on structured follow-ups to adjust and sustain progress.
Key takeaway: Effective programs evolve with the client, empowering them to build skills and ownership. The true marker of success is sustainable results—not just weight loss, but a healthier relationship with food and lifelong habits.
Study Guide – Chapter 23: Special Diet Scenarios
Introduction
Special diet scenarios require adapting nutrition strategies for people with chronic diseases or unique life stages. This chapter highlights evidence-based approaches for cardiovascular disease, diabetes, pregnancy, older adults, and youth—each with distinct nutritional priorities .
Cardiovascular Disease (CVD)
Key Diets
- Mediterranean Diet: Plant-based, rich in olive oil, legumes, whole grains, nuts, fruits, vegetables, and fish. Benefits: ↓ LDL, ↓ inflammation, ↓ risk of heart attack/stroke (~30% in PREDIMED trial) .
- DASH Diet: Emphasizes fruits, vegetables, whole grains, low-fat dairy, lean proteins, and limited sodium. Benefits: ↓ systolic BP by 5–11 mmHg .
Other Strategies
- Replace saturated with unsaturated fats; avoid trans fats.
- Plant-based diets lower cholesterol/BP but may need B12, iron, omega-3 supplements .
- Weight loss (5–10%) improves cholesterol, BP, and blood sugar .
- Limit cholesterol-rich foods (esp. for those with diabetes/CVD).
Summary: A heart-healthy diet = plant-forward, fiber-rich, with unsaturated fats, while limiting saturated fat, sodium, added sugar, and processed foods .
Diabetes
Core Nutrition Strategies
- Carbohydrate Management
- Favor high-fiber carbs: whole grains, legumes, fruits, vegetables.
- Aim for 25–35g fiber/day.
- Avoid refined carbs, soda, and sweets.
- Use carb counting or plate method for portion control.
- Even carb distribution across the day; avoid heavy carb-only meals .
- Macronutrient Balance
- Protein: 15–25% of calories (lean meats, tofu, legumes).
- Fat: 30–40%, mostly unsaturated (olive oil, nuts, avocado). Avoid trans fats .
- Weight Management
- 5–10% weight loss significantly improves insulin sensitivity and A1c.
- Use portion control, journaling, smaller plates. Combine with activity (30 min brisk walking most days) .
- Flexible Eating Patterns
- Mediterranean: lowers A1c & CV risk.
- Plant-based: improves insulin sensitivity.
- Low-carb: may help, but avoid nutrient gaps.
- Low GI: lowers post-meal spikes; quality + amount of carbs still most important .
Summary: Diabetes nutrition = fiber-rich carbs, lean protein, healthy fats, limited refined foods, consistent meals, hydration, and activity .
Pregnancy
Macronutrients & Calories
- Energy: +340 kcal/day in 2nd trimester; +450 kcal/day in 3rd (small snack increase, not “eating for two”).
- Protein: ~71 g/day (extra 1–2 servings protein foods).
- Fats: Focus on DHA omega-3s (fish, algae supplements); avoid trans fats .
- Carbs: Emphasize fiber-rich whole foods; spread intake evenly, esp. for gestational diabetes .
Key Micronutrients
- Folate: 400–600 mcg/day (supplement + leafy greens, beans).
- Iron: 27 mg/day (meat, beans + vitamin C for absorption).
- Calcium: 1,000 mg/day (dairy, fortified foods).
- Vitamin D: 600 IU/day; often needs supplements.
- Iodine: 220 mcg/day (iodized salt, seafood).
- Choline: 450 mg/day (eggs, meat, supplements).
- B12: Vegans need fortified foods/supplements .
Special Considerations
- Weight gain: 25–35 lbs (varies by BMI).
- Food safety: Avoid alcohol, high-mercury fish, raw/undercooked foods, unpasteurized products. Limit caffeine to 200 mg/day .
- Nausea/heartburn/constipation: Small meals, ginger, fiber, fluids.
Summary: Balanced diet + prenatal vitamins + safe food practices = healthy pregnancy .
Older Adults
Key Needs
- Calories: Lower due to reduced metabolism, but nutrient density must rise.
- Protein: 1.0–1.2 g/kg/day to prevent sarcopenia. Spread evenly; include easy-to-chew options .
- Hydration: Encourage ~8 cups/day; thirst decreases with age.
- Fiber: 25–30 g/day for digestion and blood sugar control.
- Bone Health: Calcium 1,200 mg/day; Vitamin D 800 IU/day.
- B12: Absorption declines; fortified foods/supplements needed .
Other Considerations
- Appetite changes → small, frequent meals.
- Food security challenges → connect with programs (Meals on Wheels).
- Oral nutrition supplements may be needed.
- Chronic conditions (HTN, diabetes, kidney issues) require tailored diets .
Summary: Quality > quantity: focus on protein, calcium, vitamin D, B12, fluids, and nutrient-dense foods .
Youth (Children & Adolescents)
Needs
- Protein & Calories: High demands during growth, esp. puberty.
- Calcium & Vitamin D: 1,300 mg Ca/day + 600 IU D/day.
- Iron: 11 mg/day for boys, 15 mg/day for girls.
- Fiber: 14 g per 1,000 kcal (≈20–30 g/day). Many kids fall short .
Challenges
- Excess added sugar, sodium, and processed foods.
- Childhood obesity: ~1 in 5 U.S. kids. Solutions = daily activity, whole foods, limiting sugary drinks, smaller portions .
- Adolescents: Peer pressure, body image, fad diets → risk of nutrient gaps or disordered eating. Support with balanced, flexible approaches .
- Allergies/special diets: With planning, kids can thrive (fortified alternatives, B12 for vegetarians/vegans).
Summary: Youth nutrition should emphasize whole foods, bone growth nutrients, and healthy habits. Focus on health, energy, and development—not strict dieting .
Conclusion
Special diet scenarios demand personalized, evidence-based approaches. From CVD and diabetes management to pregnancy, older adults, and youth, nutrition plays a crucial role in preventing disease, supporting development, and promoting lifelong health.
Study Guide – Chapter 24: Extreme Fat Loss Strategies and Concerns
Introduction
Extreme fat loss methods promise rapid results but carry serious metabolic, psychological, and health risks. While attractive for aesthetics, performance, or quick weight reduction, they often lead to rebound weight gain, muscle loss, hormonal disruption, and long-term damage .
Common Extreme Fat Loss Strategies
1. Severe Caloric Restriction
- Approach: Extreme deficits, often below BMR.
- Effects: Initial rapid weight loss.
- Concerns:
- Metabolic adaptation (“starvation mode”).
- Hormonal shifts (↓ leptin, thyroid hormones).
- High muscle and nutrient loss risk .
2. Very Low-Carbohydrate Diets (Keto, Atkins, Paleo)
- Push body into ketosis (<50 g carbs/day).
- Benefits: Rapid early weight loss, reduced insulin.
- Risks: Nutrient deficiencies (B vitamins, calcium, magnesium), constipation, fatigue, potential muscle breakdown, and rebound weight regain once carbs return .
3. Intermittent/Extended Fasting
- IF (16:8, alternate-day): Moderate protocols may improve insulin sensitivity.
- Extended fasting (>24–48 hrs): Dangerous.
- Risks:
- Hypoglycemia.
- Electrolyte imbalances → arrhythmias.
- Lean mass loss without protein intake .
4. Fat-Burning Supplements/Pharmaceuticals
- Supplements: Caffeine, herbal stimulants, appetite suppressants (often unregulated).
- Drugs: Orlistat, Phentermine, GLP-1 agonists (semaglutide).
- Risks:
- Heart issues, digestive distress, vitamin malabsorption.
- Dependency and rebound hunger/weight after discontinuation .
5. Extreme Exercise Regimens
- Multiple daily HIIT sessions or ultra-endurance training.
- Risks:
- Overtraining syndrome (fatigue, suppressed immunity, mood changes).
- Muscle catabolism.
- Injury risk (stress fractures, tendonitis).
- Potential RED-S (Relative Energy Deficiency in Sport) .
The infographic on page 6 summarizes these four categories with risks: caloric restriction, VLCDs, fasting, and supplements .
Health Consequences
Muscle Loss
- 20–40% of weight lost in extreme diets may be from muscle.
- Reduces metabolism, strength, and long-term weight maintenance .
Hormonal Dysregulation
- ↓ Thyroid → fatigue, cold sensitivity.
- ↓ Leptin & ↑ Ghrelin → more hunger, less satiety.
- ↓ Testosterone/Estrogen → reduced libido, fertility issues, bone loss.
- ↑ Cortisol → worsens muscle breakdown and sleep issues .
Psychological Effects
- Higher risk of depression, anxiety, binge-restrict cycles, eating disorders.
- Social withdrawal from fear of eating situations .
Cardiovascular/Other Risks
- Electrolyte imbalance → arrhythmias.
- Hypotension → dizziness/fainting.
- Gallstones from rapid fat loss .
- Kidney/liver strain.
The chart on page 9 clearly links physiological risks (muscle loss, metabolic adaptation, nutrient deficiencies, cardiovascular stress) with psychological effects and long-term yo-yo dieting .
Sustainable Alternatives
- Moderate caloric deficits (300–500 kcal/day): Yields ~1–2 lbs/week loss.
- Adequate protein (1.2–2.0 g/kg): Protects lean mass.
- Resistance training (2–3x/week): Preserves muscle and metabolism.
- Balanced macros: Include whole carbs, lean protein, healthy fats.
- Behavioral support: Mindful eating, stress/sleep management, social support, food tracking .
As shown on page 11, sustainable methods lead to gradual weight loss with muscle preservation, avoiding hormonal disruption .
Disordered Eating Concerns
Red Flags
- Extreme guilt after meals.
- Skipping meals routinely.
- Obsessive body checking.
- Fear of weight gain despite low weight .
Referral Pathways
- Registered Dietitians (specialized in EDs).
- Therapists/Psychologists (CBT, family therapy).
- Physicians/Psychiatrists (medical/medication support).
- Organizations: NEDA, AND, IAEDP provide directories/resources .
Coaching Considerations
- Educate on safe practices: Promote slow weight loss (0.5–1% body weight/week).
- Address behavior challenges: Build positive relationship with food/body image; emphasize gradual habit change.
- Encourage holistic health: Stress management, adequate sleep, balanced activity. Watch for burnout or disordered eating signs .
Conclusion
Extreme fat loss may deliver rapid results but undermines metabolism, hormones, mental health, and long-term sustainability. Sustainable, evidence-based practices—moderate deficits, protein, resistance training, and holistic behavior strategies—are far safer and more effective for lasting success.
Study Guide – Chapter 25: Building a Nutrition Coaching Business
Introduction
The nutrition coaching industry is expanding rapidly due to demand for personalized health guidance. Building a successful business requires nutrition expertise + strategic planning + business acumen. This chapter outlines how to establish, grow, and scale a thriving practice .
Defining Vision and Mission
- Vision: Long-term impact (e.g., “empowering busy professionals to eat well and reduce disease risk”).
- Mission: Purpose and daily objectives (e.g., “deliver personalized coaching rooted in science and behavior change”).
- A clear vision/mission:
- Guides branding, services, and marketing.
- Builds client and stakeholder trust.
- Supports long-term consistency .
Creating a Business Plan
Entrepreneurs with formal plans are nearly twice as likely to succeed. A strong plan includes :
- Executive Summary – Big-picture vision, target market, financial snapshot.
- Market Analysis – Competitors, demographics, demand.
- Services/Products – Programs, packages, pricing, uniqueness.
- Marketing/Sales Strategy – How to attract and convert clients.
- Financial Projections – Costs, revenue streams, break-even analysis.
A business plan serves as a roadmap and should be revisited regularly as markets change.
Market Positioning and Niches
- The field is diverse: weight loss, sports nutrition, gut health, women’s health, family nutrition, bodybuilding, plant-based eating (see popular niches chart on page 5).
- Specialization helps credibility and attracts ideal clients.
- Use SWOT analysis (Strengths, Weaknesses, Opportunities, Threats) to find your edge .
Marketing and Client Acquisition
Key Channels
- Social Media Engagement: Share tips, recipes, testimonials, Q&A sessions.
- Content Marketing: Blogs, newsletters, podcasts, YouTube. Boosts SEO and builds authority.
- Referral Programs: Reward satisfied clients for bringing new ones.
- Strategic Partnerships: Work with gyms, clinics, or wellness centers for referrals.
Retention Strategies
- Personalize Plans – Tailored to lifestyle and culture.
- Track Progress – Regular monitoring and celebrating wins.
- Clear Communication – Set expectations, show empathy, maintain confidentiality.
- Build Community – Group calls, private forums, or social media groups for support .
Operational Models
Common structures :
- One-on-One Coaching: Premium, personalized, but time-limited.
- Group Coaching: Efficient, affordable, adds peer support.
- Subscription Services: Recurring income (meal plans, group calls, exclusive content).
- Corporate Wellness: Seminars, workshops, or employer-funded coaching.
Most businesses mix models for scalability (e.g., 1:1 coaching + online groups + occasional workshops).
Leveraging Technology
Digital tools enhance efficiency and scale :
- Apps: Tracking (MyFitnessPal, Cronometer), custom coaching platforms.
- Scheduling Tools: Calendly, Acuity, CRMs for client management and payments.
- Wearables: Monitor activity, sleep, biometrics.
- Online Coaching: Video calls, webinars, online courses expand global reach.
Research shows online coaching can equal or outperform in-person due to convenience and adherence (see funnel graphic on page 13).
Scaling the Business
- Delegation: Hire assistants for admin, marketing, or content. Outsource to specialists.
- Hiring Coaches: Use SOPs for onboarding and consistency.
- Partnerships: With trainers, therapists, or doctors for broader services.
- Service Diversification: Add courses, group programs, or workplace wellness.
Scale thoughtfully: prioritize quality, start small, and expand with demand and revenue .
Continuous Education and Adaptation
- Stay updated with nutrition science, certifications, and coaching techniques.
- Attend workshops, read journals, join professional groups.
- Adapt services to client demand (e.g., plant-based, gut health, diabetes).
- Respond to industry changes—COVID-19 accelerated the move to virtual coaching .
Conclusion
A thriving nutrition coaching business blends passion, expertise, strategy, and adaptability:
- Define vision and mission.
- Build a clear business plan and niche.
- Market effectively and retain clients through trust and personalization.
- Use tech and diverse business models to scale.
- Continue learning and adapting to industry shifts.
Key takeaway: Success comes from combining nutrition knowledge with entrepreneurial skills, creating not just a business but a sustainable practice that positively impacts lives.
Study Guide – Chapter 26: Legal and Ethical Concerns as a Nutrition Coach
Introduction
Nutrition coaches operate in a complex legal and ethical environment. Unlike registered dietitians, their role is not standardized by law, and regulations vary by state or country. Understanding scope of practice, client rights, informed consent, confidentiality, and professionalism is essential for safe, effective coaching .
Scope of Practice and Legal Boundaries
- Nutrition Coaches provide general healthy eating and lifestyle education (portion control, food labels, balanced meals).
- Registered Dietitians (RDs) provide Medical Nutrition Therapy (MNT)—personalized diets for conditions like diabetes or kidney disease. Unless licensed, coaches cannot diagnose or prescribe therapeutic diets .
U.S. Laws and Regulations
- Varies by state: Some require licenses to give individualized nutrition advice (e.g., Florida), while others only protect specific titles (e.g., California).
- Virtual coaching: Coaches must follow the client’s state/country laws, not just their own .
Inside vs Outside Scope
- Inside: Basic recommendations, citing dietary guidelines, general healthy eating.
- Outside: Prescribing meal plans, treating conditions, or making disease-related claims .
Rule of thumb: Stay in your lane. Support wellness; refer clients with medical needs to RDs or doctors.
Ethical Standards
Informed Consent & Client Autonomy
- Clearly state your role: “general education, not medical advice.”
- Explain services, confidentiality, and costs before starting.
- Respect autonomy: involve clients in setting goals and let them make choices .
Confidentiality & Privacy
- Keep client information private, with limited exceptions (safety concerns, court orders).
- Use HIPAA/GDPR-compliant tools, secure storage, and get consent for sharing testimonials .
Integrity and Evidence-Based Practice
- Be honest about credentials and limits.
- Provide science-based advice, not fads or pseudoscience.
- Disclose conflicts of interest (e.g., if you earn commission on supplements).
- Maintain professional boundaries; avoid dual relationships or over-involvement .
The diagram on page 8 summarizes core principles (integrity, client-centered care, confidentiality) and ways to avoid harm (no false promises, no fad diets, always clarify scope).
Professional Guidelines and Codes of Ethics
Organizations like NANP, ISSN, ICF, NBHWC, ACSM outline shared values: honesty, competence, confidentiality, cultural sensitivity, and accountability .
Handling dilemmas:
- When pressured to act outside scope, explain limits, document the discussion, and provide a referral.
- If clients reveal risks (e.g., eating disorders, self-harm), encourage professional help and pause coaching until appropriate care is in place .
Legal Foundations for Coaching Businesses
- Certifications & Credentials – Use recognized programs (CNS, health coach). Only RDs may provide MNT.
- Liability Insurance – Protects against claims or lawsuits. Ensure it covers both in-person and online work.
- Client Agreements – Written contracts should include services, limits, payment terms, confidentiality, and liability waivers .
The checklist on page 12 highlights: Certification, Scope of Practice, Insurance, Client Agreement, HIPAA Compliance.
Ethical & Legal Challenges in Virtual Coaching
- Algorithmic Bias: AI tools may exclude cultural foods or promote unsafe advice. Coaches must review and adapt tech-based recommendations.
- Persuasive Design: Apps should nudge, not shame. Respect autonomy.
- Misinformation Risks: Always fact-check digital tool outputs.
- Jurisdiction Issues: Follow the client’s state/country laws.
- Privacy: Use secure, HIPAA-compliant tools. Document interactions carefully .
Marketing and Advertising Ethics
- Avoid false claims: Don’t guarantee outcomes or claim to treat/cure diseases. Use disclaimers (“Results may vary”).
- Transparency: Always disclose affiliations or commissions (FTC rules).
- Authenticity: Share real stories with permission. Avoid exaggerated before/after photos (page 15 chart contrasts unethical “miracle claims” vs ethical alternatives).
- Platform rules: Social media bans body-shaming or unsafe health ads—follow these for professionalism .
Common Dilemmas and Solutions
- Meal plan for diabetes? → Refer to RD.
- Supplements with little research? → Provide evidence-based info + disclaim limitations.
- AI conflicting with client goals? → Allow manual adjustments and client input.
- Extensive platform data collection? → Ensure compliance with privacy laws .
Conclusion
Legal and ethical competence is as vital as nutrition knowledge. Coaches must:
- Know their scope and local regulations.
- Gain informed consent and respect autonomy.
- Protect confidentiality and act with integrity.
- Market truthfully and avoid exaggerated claims.
- Adapt to technology while safeguarding client trust.
Key takeaway: By combining ethical integrity with legal awareness, nutrition coaches protect their clients, safeguard their careers, and strengthen the credibility of the profession.
 Have a question?
Have a question? 
Tyler Read
PTPioneer Editorial Integrity
All content published on PTPioneer is checked and reviewed extensively by our staff of experienced personal trainers, nutrition coaches, and other Fitness Experts. This is to make sure that the content you are reading is fact-checked for accuracy, contains up-to-date information, and is relevant. We only add trustworthy citations that you can find at the bottom of each article. You can read more about our editorial integrity here.